 W
WInterventional radiology (IR) is a medical subspecialty that performs various minimally-invasive procedures using medical imaging guidance, such as x-ray fluoroscopy, computed tomography, magnetic resonance imaging, or ultrasound. IR performs both diagnostic and therapeutic procedures through very small incisions or body orifices. Diagnostic IR procedures are those intended to help make a diagnosis or guide further medical treatment, and include image-guided biopsy of a tumor or injection of an imaging contrast agent into a hollow structure, such as a blood vessel or a duct. By contrast, therapeutic IR procedures provide direct treatment—they include catheter-based medicine delivery, medical device placement, and angioplasty of narrowed structures.
 W
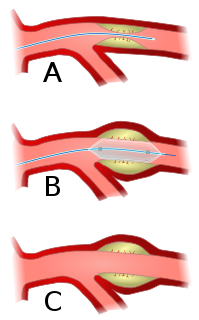
WAngioplasty, also known as balloon angioplasty and percutaneous transluminal angioplasty (PTA), is a minimally invasive endovascular procedure used to widen narrowed or obstructed arteries or veins, typically to treat arterial atherosclerosis. A deflated balloon attached to a catheter is passed over a guide-wire into the narrowed vessel and then inflated to a fixed size. The balloon forces expansion of the blood vessel and the surrounding muscular wall, allowing an improved blood flow. A stent may be inserted at the time of ballooning to ensure the vessel remains open, and the balloon is then deflated and withdrawn. Angioplasty has come to include all manner of vascular interventions that are typically performed percutaneously.
 W
WAtherectomy is a minimally invasive technique for removing atherosclerosis from blood vessels within the body. It is an alternative to angioplasty for the treatment of peripheral artery disease, but the studies that exist are not adequate to determine whether it is superior to angioplasty. It has also been used to treat coronary artery disease, albeit without evidence of superiority to angioplasty.
 W
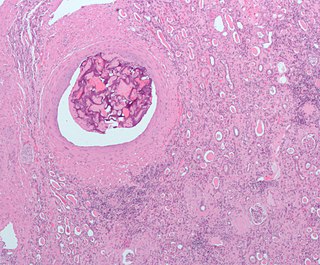
WA biopsy is a medical test commonly performed by a surgeon, interventional radiologist, or an interventional cardiologist. The process involves extraction of sample cells or tissues for examination to determine the presence or extent of a disease. The tissue is generally examined under a microscope by a pathologist; it may also be analyzed chemically. When an entire lump or suspicious area is removed, the procedure is called an excisional biopsy. An incisional biopsy or core biopsy samples a portion of the abnormal tissue without attempting to remove the entire lesion or tumor. When a sample of tissue or fluid is removed with a needle in such a way that cells are removed without preserving the histological architecture of the tissue cells, the procedure is called a needle aspiration biopsy. Biopsies are most commonly performed for insight into possible cancerous or inflammatory conditions.
 W
WCryoablation is a process that uses extreme cold to destroy tissue. Cryoablation is performed using hollow needles (cryoprobes) through which cooled, thermally conductive, fluids are circulated. Cryoprobes are positioned adjacent to the target in such a way that the freezing process will destroy the diseased tissue. Once the probes are in place, the attached cryogenic freezing unit removes heat from ("cools") the tip of the probe and by extension from the surrounding tissues.
 W
WEmbolization refers to the passage and lodging of an embolus within the bloodstream. It may be of natural origin (pathological), in which sense it is also called embolism, for example a pulmonary embolism; or it may be artificially induced (therapeutic), as a hemostatic treatment for bleeding or as a treatment for some types of cancer by deliberately blocking blood vessels to starve the tumor cells.
 W
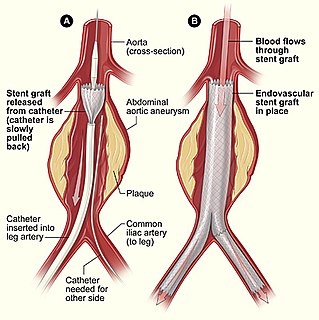
WEndovascular aneurysm repair (EVAR), is a type of minimally-invasive endovascular surgery used to treat pathology of the aorta, most commonly an abdominal aortic aneurysm (AAA). When used to treat thoracic aortic disease, the procedure is then specifically termed TEVAR for "thoracic endovascular aortic/aneurysm repair." The procedure involves the placement of an expandable stent graft within the aorta to treat aortic disease without operating directly on the aorta. In 2003, EVAR surpassed open aortic surgery as the most common technique for repair of AAA, and in 2010, EVAR accounted for 78% of all intact AAA repair in the United States.
 W
WEndovascular coiling is an endovascular treatment for intracranial aneurysms and bleeding throughout the body. The procedure reduces blood circulation to the aneurysm through the use of microsurgical detachable platinum wires, with the clinician inserting one or more into the aneurysm until it is determined that blood flow is no longer occurring within the space. It is one of two main treatments for cerebral aneurysms, the other being surgical clipping. Clipping is an alternative to stenting for bleeding.
 W
WEthylene vinyl alcohol (EVOH) is a formal copolymer of ethylene and vinyl alcohol. Because the latter monomer mainly exists as its tautomer acetaldehyde, the copolymer is prepared by polymerization of ethylene and vinyl acetate to give the ethylene vinyl acetate (EVA) copolymer followed by hydrolysis. EVOH copolymer is defined by the mole % ethylene content: lower ethylene content grades have higher barrier properties; higher ethylene content grades have lower temperatures for extrusion.
 W
WAn inferior vena cava filter is a type of vascular filter, a medical device that is implanted by vascular surgeons or interventional radiologists into the inferior vena cava to prevent life-threatening pulmonary emboli (PEs). Their effectiveness and safety profile is well established. In cases where patients are at high risk of developing a clinically significant PE and cannot be sufficiently anticoagulated, placement of an IVC filter may be recommended.
 W
WA nephrostomy is an artificial opening created between the kidney and the skin which allows for the urinary diversion directly from the upper part of the urinary system.
 W
WParacentesis is a form of body fluid sampling procedure, generally referring to peritoneocentesis in which the peritoneal cavity is punctured by a needle to sample peritoneal fluid.
 W
WRadiofrequency ablation (RFA), also called fulguration, is a medical procedure in which part of the electrical conduction system of the heart, tumor or other dysfunctional tissue is ablated using the heat generated from medium frequency alternating current. RFA is generally conducted in the outpatient setting, using either local anesthetics or conscious sedation anesthesia. When it is delivered via catheter, it is called radiofrequency catheter ablation.
 W
WThe Seldinger technique, also known as Seldinger wire technique, is a medical procedure to obtain safe access to blood vessels and other hollow organs. It is named after Dr. Sven Ivar Seldinger (1921–1998), a Swedish radiologist who introduced the procedure in 1953.
 W
WSelective internal radiation therapy (SIRT), also known as transarterial radioembolization (TARE), radioembolization or intra-arterial microbrachytherapy is a form of radiation therapy used in interventional radiology to treat cancer. It is generally for selected patients with surgically unresectable cancers, especially hepatocellular carcinoma or metastasis to the liver. The treatment involves injecting tiny microspheres of radioactive material into the arteries that supply the tumor, where the spheres lodge in the small vessels of the tumor. Because this treatment combines radiotherapy with embolization, it is also called radioembolization. The chemotherapeutic analogue is called chemoembolization, of which transcatheter arterial chemoembolization (TACE) is the usual form.
 W
WIn medicine, a stent is a metal or plastic tube inserted into the lumen of an anatomic vessel or duct to keep the passageway open, and stenting is the placement of a stent. There is a wide variety of stents used for different purposes, from expandable coronary, vascular and biliary stents, to simple plastic stents used to allow the flow of urine between kidney and bladder. "Stent" is also used as a verb to describe the placement of such a device, particularly when a disease such as atherosclerosis has pathologically narrowed a structure such as an artery.
 W
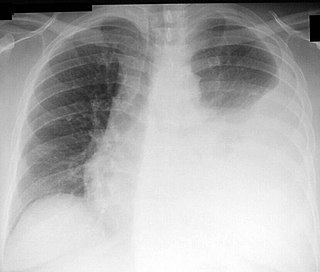
WThoracentesis, also known as thoracocentesis, pleural tap, needle thoracostomy, or needle decompression is an invasive medical procedure to remove fluid or air from the pleural space for diagnostic or therapeutic purposes. A cannula, or hollow needle, is carefully introduced into the thorax, generally after administration of local anesthesia. The procedure was first performed by Morrill Wyman in 1850 and then described by Henry Ingersoll Bowditch in 1852.
 W
WTransjugular intrahepatic portosystemic shunt is an artificial channel within the liver that establishes communication between the inflow portal vein and the outflow hepatic vein. It is used to treat portal hypertension which frequently leads to intestinal bleeding, life-threatening esophageal bleeding and the buildup of fluid within the abdomen (ascites).
 W
WUterine artery embolization is a procedure in which an interventional radiologist uses a catheter to deliver small particles that block the blood supply to the uterine body. The procedure is done for the treatment of uterine fibroids and adenomyosis. This minimally invasive procedure is commonly used in the treatment of uterine fibroids and is also called uterine fibroid embolization.