 W
WMedicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance Association of America describes Medicaid as "a government insurance program for persons of all ages whose income and resources are insufficient to pay for health care."
 W
WMedicare is a national health insurance program in the United States, begun in 1966 under the Social Security Administration (SSA) and now administered by the Centers for Medicare and Medicaid Services (CMS). It primarily provides health insurance for Americans aged 65 and older, but also for some younger people with disability status as determined by the Social Security Administration, as well as people with end stage renal disease and amyotrophic lateral sclerosis.
 W
WOregon ballot measure 44 was an initiated state statute ballot measure on the November 7, 2006 general election ballot. The Measure modified the eligibility requirements for Oregon residents to participate in the Oregon Prescription Drug Program. The program intends to make prescription drugs available to participants at the lowest possible cost through negotiated price discounts. It was passed overwhelmingly by voters, garnering 78% of the vote.
 W
WAllion Healthcare (NASDAQ: ALLI) was the parent company of MOMSpharmacy based in Melville, New York primarily known for providing mail order HIV medications to patients who are primarily on Medicaid or the AIDS Drug Assistance Program (ADAP).
 W
WCareSource is a nonprofit that began as a managed health care plan serving Medicaid members in Ohio. Today, it provides public health care programs including Medicaid, Medicare, and Marketplace. The company is headquartered in Dayton, Ohio. It is the largest Medicaid plan in Ohio and is second in the United States. Its tag line is Healthcare with Heart. In 2019, CareSource earned one of the top spots for quality according to 2019 Ohio Department of Medicaid (ODM) Managed Care Plans Report Card.
 W
WThe Centers for Medicare & Medicaid Services (CMS), is a federal agency within the United States Department of Health and Human Services (HHS) that administers the Medicare program and works in partnership with state governments to administer Medicaid, the Children's Health Insurance Program (CHIP), and health insurance portability standards. In addition to these programs, CMS has other responsibilities, including the administrative simplification standards from the Health Insurance Portability and Accountability Act of 1996 (HIPAA), quality standards in long-term care facilities through its survey and certification process, clinical laboratory quality standards under the Clinical Laboratory Improvement Amendments, and oversight of HealthCare.gov. CMS was previously known as the Health Care Financing Administration (HCFA) until 2001.
 W
WThe Children's Health Insurance Program (CHIP) – formerly known as the State Children's Health Insurance Program (SCHIP) – is a program administered by the United States Department of Health and Human Services that provides matching funds to states for health insurance to families with children. The program was designed to cover uninsured children in families with incomes that are modest but too high to qualify for Medicaid. The program was passed into law as part of the Balanced Budget Act of 1997, and the statutory authority for CHIP is under title XXI of the Social Security Act.
 W
WCovered California is the health insurance marketplace in the U.S. state of California established under the federal Patient Protection and Affordable Care Act (ACA). The exchange enables eligible individuals and small businesses to purchase private health insurance coverage at federally subsidized rates. It is administered by an independent agency of the government of California.
 W
WElderly care, or simply eldercare, is the fulfillment of the special needs and requirements that are unique to senior citizens. This broad term encompasses such services as assisted living, adult day care, long term care, nursing homes, hospice care, and home care. Because of the wide variety of elderly care found nationally, as well as differentiating cultural perspectives on elderly citizens, it cannot be limited to any one practice. For example, many countries in Asia use government-established elderly care quite infrequently, preferring the traditional methods of being cared for by younger generations of family members.
 W
WThe Fairness Project is a United States 501(c)(4) charitable organization created in October 2015. They promote general economic and social justice throughout the US by the use of ballot measures to circumvent deadlocks in law changes by the legislative and executive branches of government. They act as a national body by supporting state organizations and campaigns with targeted funding rather than by direct campaigning. They support the gathering of signatures to meet the variable requirements to trigger ballots in states and then aid the campaigns with early financial backing, strategic advice, and various campaign tools.
 W
WThe Federal Insurance Contributions Act is a United States federal payroll contribution directed towards both employees and employers to fund Social Security and Medicare—federal programs that provide benefits for retirees, people with disabilities, and children of deceased workers.
 W
WThe Health Insurance Portability and Accountability Act of 1996 is a United States federal statute enacted by the 104th United States Congress and signed into law by President Bill Clinton on August 21, 1996. It was created primarily to modernize the flow of healthcare information, stipulate how personally identifiable information maintained by the healthcare and healthcare insurance industries should be protected from fraud and theft, and address limitations on healthcare insurance coverage.
 W
WHome care is supportive care provided in the home. Care may be provided by licensed healthcare professionals who provide medical treatment needs or by professional caregivers who provide daily assistance to ensure the activities of daily living (ADLs) are met. In-home medical care is often and more accurately referred to as home health care or formal care. Often, the term home health care is used to distinguish it from non-medical care, custodial care, or private-duty care which refers to assistance and services provided by persons who are not nurses, doctors, or other licensed medical personnel. For terminally ill patients, home care may include hospice care. For patients recovering from surgery or illness, home care may include rehabilitative therapies.
 W
WThe Improving Medicare Post-Acute Care Transformation Act of 2014 or IMPACT Act of 2014 is a bill that is intended to change and improve Medicare's post-acute care (PAC) services and how they are reported.
 W
WA Katie Beckett waiver or TEFRA waiver is a Medicaid waiver concerning the income eligibility for home-based Medicaid services for children under the age of nineteen. Prior to the Katie Beckett waiver, if a child with significant medical needs received treatment at home, all of the financial resources of the parents would be "deemed" as the income of the child for the purposes of determining Medicaid eligibility. Only after a hospitalization lasting more than thirty days would the parents' income no longer be deemed to the child, allowing the child to then qualify for Medicaid coverage. The effect was that many families, unable to afford home treatment, kept their children in costly hospital settings in order to meet the Medicaid 30-day requirement. Katie Beckett waivers allow Medicaid to cover medical services for children in the home, regardless of the parents' income, in cases where home-based treatment will cost less than or the same as treatment in a hospital.
 W
WLong-term care (LTC) is a variety of services which help meet both the medical and non-medical needs of people with a chronic illness or disability who cannot care for themselves for long periods. Long term care is focused on individualized and coordinated services that promote independence, maximize patients' quality of life, and meet patients' needs over a period of time.
 W
WMark Barr McClellan is the director of the Robert J Margolis Center for Health Policy and the Margolis Professor of Business, Medicine and Health Policy at Duke University. Formerly, he was a senior fellow and director of the Health Care Innovation and Value Initiative at the Engelberg Center for Health Care Reform at The Brookings Institution, in Washington, D.C. McClellan served as commissioner of the United States Food and Drug Administration under President George W. Bush from 2002 through 2004, and subsequently as administrator of the Centers for Medicare and Medicaid Services from 2004 through 2006.
 W
WIn the United States, the Medicaid coverage gap refers to the group of uninsured people who are both ineligible for Medicaid under its previous rules, which still apply in these states, and too poor to qualify for the ACA's subsidies and credits that were designed to allow middle-class Americans to purchase health insurance. The number of Americans in this gap has been estimated to be almost 3 million as of January 2016, according to the Kaiser Family Foundation. The Foundation has also said that 90% of the people in this gap live in the South. In states that have not expanded Medicaid, eligibility requirements for Medicaid are limited to parents making 44% or less of the poverty line, and in almost all such states, all adults without children are ineligible. The coverage gap results from this and a number of factors, such as the fact that the ACA was designed so that the poor would receive coverage through Medicaid and so did not include an alternative program for them. For example, as of April 2014, someone living in Texas, a nonexpansion state, had to be making less than $3,737 per year to be eligible for Medicaid, and had to make at least $11,490 or $23,550 to be eligible for ACA subsidies. On November 1, 2015, an episode of Last Week Tonight with John Oliver dedicated its main segment to discussing the Medicaid coverage gap.
 W
WHome and Community-Based Services waivers or Section 1915(c) waivers, 42 U.S.C. Ch. 7, § 1396n §§ 1915(c), are a type of Medicaid waiver. HCBS waivers expand the types of settings in which people can receive comprehensive long-term care under Medicaid. Prior to the creation of HCBS waivers, comprehensive long-term care was available through Medicaid only in institutional settings. Under an HCBS waiver, states can use Medicaid funds to provide a broad array of non-medical services not otherwise covered by Medicaid, if those services allow recipients to receive care in community and residential settings as an alternative to institutionalization.
 W
WThe Medicare and Medicaid Extenders Act of 2010 is a federal law of the United States, enacted in 2010. The law was first introduced into the House as H.R. 4994 on April 13, 2010 by Rep. John Lewis (D-GA) with 20 cosponsors. It was then referred to the House Committee on Ways and Means and the House Committee on the Budget.
 W
WThe Medicare Fraud Strike Force is a multi-agency team of United States federal, state, and local investigators who combat Medicare fraud through data analysis and increased community policing. Launched in 2007, the Strike Force is coordinated by the United States Department of Justice and the Department of Health and Human Services. It combines the data-analysis capabilities of the Centers for Medicare and Medicaid Services, the investigative resources of the FBI, and the prosecutorial resources of the Department of Justice and the U.S. Attorneys' Offices.
 W
WThe Medicare Prescription Drug, Improvement, and Modernization Act, also called the Medicare Modernization Act or MMA, is a federal law of the United States, enacted in 2003. It produced the largest overhaul of Medicare in the public health program's 38-year history.
 W
WThe Medicare, Medicaid, and SCHIP Balanced Budget Refinement Act of 1999 is a federal law of the United States, enacted in 1999. The BBRA was first introduced into the House as H.R. 3075 on October 14, 1999 by Rep. William M. Thomas (R-CA) with 75 cosponsors. It was read twice and then referred to the Senate Committee on Finance. The bill was then slightly altered and reintroduced by Thomas as H.R. 3426 on November 17, 1999. After referral to the House committees on Ways and Means and Commerce, it was incorporated by cross-reference in the conference report into H.R. 3194 on November 18, 1999. The H.R. 3194 bill had been introduced by Rep. Ernest J. Istook, Jr. (R-OK) on November 2, 1999, and was enacted with official title: Making consolidated appropriations for the fiscal year ending September 30, 2000, and for other purposes. The State Health Insurance Trial was administered by the United States Department of Health and Human Services.
 W
WThe Omnibus Budget Reconciliation Act of 1987 was federal law that was enacted by the 100th United States Congress and signed into law by President Ronald Reagan.
 W
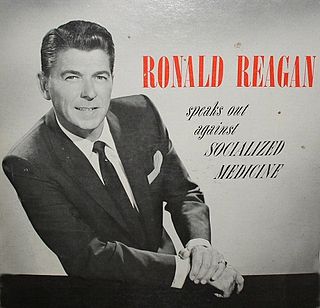
WOperation Coffee Cup was a campaign conducted by the American Medical Association (AMA) during the late 1950s and early 1960s in opposition to the Democrats' plans to extend Social Security to include health insurance for the elderly, later known as Medicare. As part of the plan, doctors' wives would organize coffee meetings in an attempt to convince acquaintances to write letters to Congress opposing the program. The operation received support from Ronald Reagan, who in 1961 produced the LP record Ronald Reagan Speaks Out Against Socialized Medicine for the AMA, outlining arguments against what he called socialized medicine. This record would be played at the coffee meetings.
 W
WMedicare Part D, also called the Medicare prescription drug benefit, is an optional United States federal-government program to help Medicare beneficiaries pay for self-administered prescription drugs through prescription drug insurance premiums. Part D was originally proposed by President Bill Clinton in 1999, then by both political parties and Houses of Congress and President Bush during 2002 and 2003. The final bill was enacted as part of the Medicare Modernization Act of 2003 and went into effect on January 1, 2006. The various proposals were substantially alike in that Part D was optional, it was separated from the other three Parts of Medicare in most proposals, and it used private pharmacy benefit managers on a regional basis to negotiate drug prices. The differences included consistent benefits nationwide in the Clinton/Democratic proposals and a wide array of deductibles and co-pays ; Bush's initial proposal included true catastrophic coverage for middle income seniors, but it was not in the final version and is a feature still not available in Part D.
 W
WThe proposed Public Option Act is a bill that was introduced to the United States House of Representatives in 2010. It would permit U.S. citizens to buy into Medicare public health insurance by paying premiums. The bill was introduced by Representative Alan Grayson, a Democrat from Florida. As of March 24, 2010 it had eighty cosponsors.
 W
WThe U.S. Railroad Retirement Board (RRB) is an independent agency in the executive branch of the United States government created in 1935 to administer a social insurance program providing retirement benefits to the country's railroad workers.
 W
WA rural health clinic (RHC) is a clinic located in a rural, medically under-served area in the United States that has a separate reimbursement structure from the standard medical office under the Medicare and Medicaid programs. RHCs were established by the Rural Health Clinic Services Act of 1977, . The RHC program increases access to health care in rural areas bycreating special reimbursement mechanisms that allow clinicians to practice in rural, under-served areas increasing utilization of physician assistants (PA) and nurse practitioners (NP)
 W
WThomas Andrew Scully is an American lawyer and former government official. He was the Administrator of the Centers for Medicare and Medicaid Services (CMS) from 2001 to 2004 under President George W. Bush. Scully currently is a Principal at Lincoln Policy Group and a partner at its affiliated law firm Scully, Roskey & Missmar, where he focuses on health care regulatory and legislative matters, as well as on advising clients on health policy and strategies for health care delivery. Scully is also a general partner at Welsh, Carson, Anderson & Stowe, a private equity investment firm, where he focuses on health care investments.
 W
WThe Social Security Amendments of 1965, Pub.L. 89–97, 79 Stat. 286, enacted July 30, 1965, was legislation in the United States whose most important provisions resulted in creation of two programs: Medicare and Medicaid. The legislation initially provided federal health insurance for the elderly and for poor families.
 W
WSupplemental needs trust is a US-specific term for a type of special needs trust. Supplemental needs trusts are compliant with provisions of US state and federal law and are designed to provide benefits to, and protect the assets of, individuals with physical, psychiatric, or intellectual disabilities, and still allow such persons to be qualified for and receive governmental health care benefits, especially long-term nursing care benefits, under the Medicaid welfare program.
 W
WThe Expanded and Improved Medicare for All Act, also known as Medicare for All or United States National Health Care Act, is a bill first introduced in the United States House of Representatives by former Representative John Conyers (D-MI) in 2003, with 25 cosponsors. As of September 26, 2017, it had 120 cosponsors, a majority of Democrats in the House of Representatives, and the highest level of support the bill has received since Conyers began annually introducing the bill in 2003. As of December 6, 2018, the bill's cosponsors had increased to 124.