 W
WThe cranial nerve exam is a type of neurological examination. It is used to identify problems with the cranial nerves by physical examination. It has nine components. Each test is designed to assess the status of one or more of the twelve cranial nerves (I-XII). These components correspond to testing the sense of smell (I), visual fields and acuity (II), eye movements and pupils, sensory function of face (V), strength of facial (VII) and shoulder girdle muscles (XI), hearing, taste, pharyngeal movement and reflex, tongue movements (XII).
 W
WDeep brain stimulation (DBS) is a neurosurgical procedure involving the placement of a medical device called a neurostimulator, which sends electrical impulses, through implanted electrodes, to specific targets in the brain for the treatment of movement disorders, including Parkinson's disease, essential tremor, and dystonia. While its underlying principles and mechanisms are not fully understood, DBS directly changes brain activity in a controlled manner.
 W
WElectrical brain stimulation (EBS), also referred to as focal brain stimulation (FBS), is a form of electrotherapy and technique used in research and clinical neurobiology to stimulate a neuron or neural network in the brain through the direct or indirect excitation of its cell membrane by using an electric current. It is used for research or for therapeutic purposes.
 W
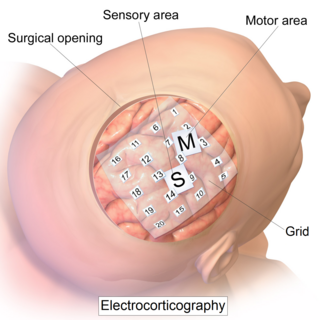
WElectrocorticography (ECoG), or intracranial electroencephalography (iEEG), is a type of electrophysiological monitoring that uses electrodes placed directly on the exposed surface of the brain to record electrical activity from the cerebral cortex. In contrast, conventional electroencephalography (EEG) electrodes monitor this activity from outside the skull. ECoG may be performed either in the operating room during surgery or outside of surgery. Because a craniotomy is required to implant the electrode grid, ECoG is an invasive procedure.
 W
WElectromyography (EMG) is an electrodiagnostic medicine technique for evaluating and recording the electrical activity produced by skeletal muscles. EMG is performed using an instrument called an electromyograph to produce a record called an electromyogram. An electromyograph detects the electric potential generated by muscle cells when these cells are electrically or neurologically activated. The signals can be analyzed to detect medical abnormalities, activation level, or recruitment order, or to analyze the biomechanics of human or animal movement. In Computer Science, EMG is also used as middleware in gesture recognition towards allowing the input of physical action to a computer as a form of human-computer interaction.
 W
WEpidural steroid injection (ESI) is a technique in which corticosteroids and a local anesthetic are injected into the epidural space around the spinal cord in an effort to improve spinal stenosis, spinal disc herniation, or both. It is of benefit with a rare rate of major side effects.
 W
WGait analysis is the systematic study of animal locomotion, more specifically the study of human motion, using the eye and the brain of observers, augmented by instrumentation for measuring body movements, body mechanics, and the activity of the muscles. Gait analysis is used to assess and treat individuals with conditions affecting their ability to walk. It is also commonly used in sports biomechanics to help athletes run more efficiently and to identify posture-related or movement-related problems in people with injuries.
 W
WLumbar puncture (LP), also known as a spinal tap, is a medical procedure in which a needle is inserted into the spinal canal, most commonly to collect cerebrospinal fluid (CSF) for diagnostic testing. The main reason for a lumbar puncture is to help diagnose diseases of the central nervous system, including the brain and spine. Examples of these conditions include meningitis and subarachnoid hemorrhage. It may also be used therapeutically in some conditions. Increased intracranial pressure is a contraindication, due to risk of brain matter being compressed and pushed toward the spine. Sometimes, lumbar puncture cannot be performed safely. It is regarded as a safe procedure, but post-dural-puncture headache is a common side effect.
 W
WManagement of dyslexia depends on a multiple of variables; there is no one specific strategy or set of strategies which will work for all who have dyslexia.
 W
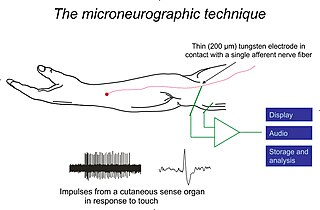
WMicroneurography is a neurophysiological method employed by scientists to visualize and record the normal traffic of nerve impulses that are conducted in peripheral nerves of waking human subjects. The method has been successfully employed to reveal functional properties of a number of neural systems, e.g. sensory systems related to touch, pain, and muscle sense as well as sympathetic activity controlling the constriction state of blood vessels. To study nerve impulses of an identified neural system, a fine tungsten needle electrode is inserted into the nerve and connected to a high gain recording amplifier. The exact position of the electrode tip within the nerve is then adjusted in minute steps until the electrode discriminates impulses of the neural system of interest. A unique feature and a significant strength of the microneurography method is that subjects are fully awake and able to cooperate in tests requiring mental attention, while impulses in a representative nerve fibre or set of nerve fibres are recorded, e.g. when cutaneous sense organs are stimulated or subjects perform voluntary precision movements.
 W
WA nerve conduction study (NCS) is a medical diagnostic test commonly used to evaluate the function, especially the ability of electrical conduction, of the motor and sensory nerves of the human body. These tests may be performed by medical specialists such as clinical neurophysiologists, physical therapists, chiropractors, physiatrists, and neurologists who subspecialize in electrodiagnostic medicine. In the United States, neurologists and physiatrists receive training in electrodiagnostic medicine as part of residency training and in some cases acquire additional expertise during a fellowship in clinical neurophysiology, electrodiagnostic medicine, or neuromuscular medicine. Outside the US, clinical neurophysiologists learn needle EMG and NCS testing.
 W
WA neurological examination is the assessment of sensory neuron and motor responses, especially reflexes, to determine whether the nervous system is impaired. This typically includes a physical examination and a review of the patient's medical history, but not deeper investigation such as neuroimaging. It can be used both as a screening tool and as an investigative tool, the former of which when examining the patient when there is no expected neurological deficit and the latter of which when examining a patient where you do expect to find abnormalities. If a problem is found either in an investigative or screening process, then further tests can be carried out to focus on a particular aspect of the nervous system.
 W
WOsmotherapy is the use of osmotically active substances to reduce the volume of intracranial contents. Osmotherapy serves as the primary medical treatment for cerebral edema. The primary purpose of osmotherapy is to improve elasticity and decrease intracranial volume by removing free water, accumulated as a result of cerebral edema, from brain's extracellular and intracellular space into vascular compartment by creating an osmotic gradient between the blood and brain. Normal serum osmolality ranges from 280-290 mOsm/kg and serum osmolality to cause water removal from brain without much side effects ranges from 300-320 mOsm/kg. Usually, 90 mL of space is created in the intracranial vault by 1.6% reduction in brain water content. Osmotherapy has cerebral dehydrating effects. The main goal of osmotherapy is to decrease intracranial pressure(ICP) by shifting excess fluid from brain. This is accomplished by intravenous administration of osmotic agents which increase serum osmolality in order to shift excess fluid from intracellular or extracellular space of the brain to intravascular compartment. The resulting brain shrinkage effectively reduces intracranial volume and decreases ICP.
 W
WRadiosurgery is surgery using radiation, that is, the destruction of precisely selected areas of tissue using ionizing radiation rather than excision with a blade. Like other forms of radiation therapy, it is usually used to treat cancer. Radiosurgery was originally defined by the Swedish neurosurgeon Lars Leksell as "a single high dose fraction of radiation, stereotactically directed to an intracranial region of interest".
 W
WRestorative neurology is a branch of neurology dedicated to improving functions of the impaired nervous system through selective structural or functional modification of abnormal neurocontrol according to underlying mechanisms and clinically unrecognized residual functions. When impaired, the body naturally reconstructs new neurological pathways and redirects activity. The field of restorative neurology works to accentuate these new pathways and primarily focuses on the theory of the plasticity of an impaired nervous system. Its main goal is to take a broken down and disordered nervous system and return it to a state of normal function. Certain treatment strategies are used to augment instead of fully replace any performance of surviving and also improving the potential of motor neuron functions. This rehabilitation of motor neurons allows patients a therapeutic approach to recovery opposed to physical structural reconstruction. It is applied in a wide range of disorders of the nervous system, including upper motor neuron dysfunctions like spinal cord injury, cerebral palsy, multiple sclerosis and acquired brain injury including stroke, and neuromuscular diseases as well as for control of pain and spasticity. Instead of applying a reconstructive neurobiological approach, i.e. structural modifications, restorative neurology relies on improving residual function. While subspecialties like neurosurgery and pharmacology exist and are useful in diagnosing and treating conditions of the nervous system, restorative neurology takes a pathophysiological approach. Instead of heavily relying on neurochemistry or perhaps an anatomical discipline, restorative neurology encompasses many fields and blends them together.
 W
WRomberg's test, Romberg's sign, or the Romberg maneuver is a test used in an exam of neurological function for balance, and also as a test for driving under the influence of an intoxicant. The exam is based on the premise that a person requires at least two of the three following senses to maintain balance while standing: proprioception ; vestibular function ; and vision.
 W
WThrombolysis, also called fibrinolytic therapy, is the breakdown (lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and in cases of severe venous thromboembolism.
 W
WTinel's sign is a way to detect irritated nerves. It is performed by lightly tapping (percussing) over the nerve to elicit a sensation of tingling or "pins and needles" in the distribution of the nerve. Percussion is usually performed moving distal to proximal. It takes its name from French neurologist Jules Tinel (1879–1952).
 W
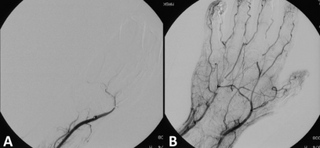
WTranscranial Doppler (TCD) and transcranial color Doppler (TCCD) are types of Doppler ultrasonography that measure the velocity of blood flow through the brain's blood vessels by measuring the echoes of ultrasound waves moving transcranially. These modes of medical imaging conduct a spectral analysis of the acoustic signals they receive and can therefore be classified as methods of active acoustocerebrography. They are used as tests to help diagnose emboli, stenosis, vasospasm from a subarachnoid hemorrhage, and other problems. These relatively quick and inexpensive tests are growing in popularity. The tests are effective for detecting sickle cell disease, ischemic cerebrovascular disease, subarachnoid hemorrhage, arteriovenous malformations, and cerebral circulatory arrest. The tests are possibly useful for perioperative monitoring and meningeal infection. The equipment used for these tests is becoming increasingly portable, making it possible for a clinician to travel to a hospital, to a doctor's office, or to a nursing home for both inpatient and outpatient studies. The tests are often used in conjunction with other tests such as MRI, MRA, carotid duplex ultrasound and CT scans. The tests are also used for research in cognitive neuroscience.
 W
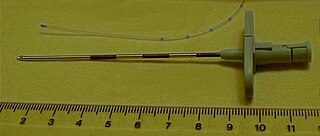
WA Tuohy (/tOO-ee/) needle is a hollow hypodermic needle, very slightly curved at the end, suitable for inserting epidural catheters.
 W
WAn upper limb neurological examination is part of the neurological examination, and is used to assess the motor and sensory neurons which supply the upper limbs. This assessment helps to detect any impairment of the nervous system, being used both as a screening and an investigative tool. The examination findings when combined with a detailed history of a patient, can help a doctor reach a specific or differential diagnosis. This would enable the doctor to commence treatment if a specific diagnosis has been made, or order further investigations if there are differential diagnoses.
 W
WVagus nerve stimulation (VNS) is a medical treatment that involves delivering electrical impulses to the vagus nerve. It is used as an add-on treatment for certain types of intractable epilepsy and treatment-resistant depression. Frequent side effects include coughing and shortness of breath. Serious side effects may include trouble talking and cardiac arrest.