 W
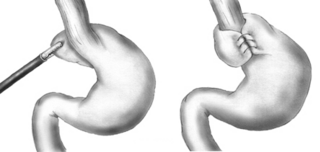
WA laparoscopic adjustable gastric band, commonly called a lap-band, A band, or LAGB, is an inflatable silicone device placed around the top portion of the stomach to treat obesity, intended to decrease food consumption.
 W
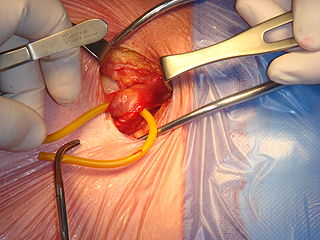
WAn appendectomy, also termed appendicectomy, is a surgical operation in which the vermiform appendix is removed. Appendectomy is normally performed as an urgent or emergency procedure to treat complicated acute appendicitis.
 W
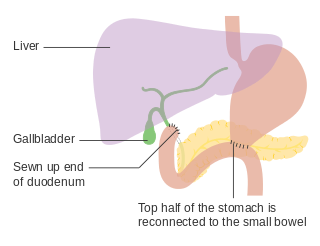
WBillroth II, more formally Billroth's operation II, is an operation in which a partial gastrectomy is performed and the cut end of the stomach is closed. The greater curvature of the stomach is then connected to the first part of the jejunum in end-to-side anastomosis. The Billroth II always follows resection of the lower part of the stomach (antrum). The surgical procedure is called a partial gastrectomy and gastrojejunostomy. The Billroth II is often indicated in refractory peptic ulcer disease and gastric adenocarcinoma.
 W
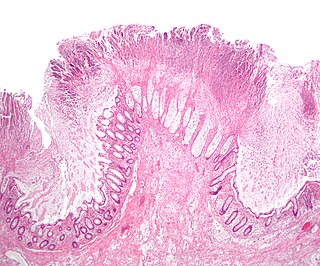
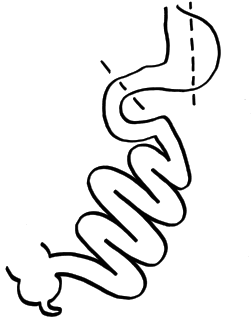
WA bowel resection or enterectomy is a surgical procedure in which a part of an intestine (bowel) is removed, from either the small intestine or large intestine. Often the word enterectomy is reserved for the sense of small bowel resection, in distinction from colectomy, which covers the sense of large bowel resection. Bowel resection may be performed to treat gastrointestinal cancer, bowel necrosis, severe enteritis, diverticular disease, Crohn's disease, endometriosis, ulcerative colitis, or bowel obstruction due to scar tissue. Other reasons to perform bowel resection include traumatic injuries and to remove polyps when polypectomy is insufficient, either to prevent polyps from ever becoming cancerous or because they are causing or threatening bowel obstruction, such as in familial adenomatous polyposis, Peutz–Jeghers syndrome, or other polyposis syndromes. Some patients require ileostomy or colostomy after this procedure as alternative means of excretion. Depending on which part and how much of the intestines are removed, there may be digestive and metabolic challenges afterward, such as short bowel syndrome.
 W
WColectomy is bowel resection of the large bowel (colon). It consists of the surgical removal of any extent of the colon, usually segmental resection. In extreme cases where the entire large intestine is removed, it is called total colectomy, and proctocolectomy denotes that the rectum is included.
 W
WColonic polypectomy is the removal of colorectal polyps in order to prevent them from turning cancerous.
 W
WA colostomy is an opening (stoma) in the large intestine (colon), or the surgical procedure that creates one. The opening is formed by drawing the healthy end of the colon through an incision in the anterior abdominal wall and suturing it into place. This opening, often in conjunction with an attached ostomy system, provides an alternative channel for feces to leave the body. Thus if the natural anus is not available for that job, an artificial anus takes over. It may be reversible or irreversible, depending on the circumstances.
 W
WIn medicine, a distal splenorenal shunt procedure (DSRS), also splenorenal shunt procedure and Warren shunt, is a surgical procedure in which the distal splenic vein is attached to the left renal vein. It is used to treat portal hypertension and its main complication. It was developed by W. Dean Warren.
 W
WEsophagectomy or oesophagectomy is the surgical removal of all or part of the esophagus.
 W
WA gastrectomy is a partial or total surgical removal of the stomach.
 W
WGastric bypass surgery refers to a surgical process in which the stomach is divided into a small upper pouch and a much larger lower "remnant" pouch and then the small intestine is rearranged to connect to both. Surgeons have developed several different ways to reconnect the intestine, thus leading to several different gastric bypass procedures (GBP). Any GBP leads to a marked reduction in the functional volume of the stomach, accompanied by an altered physiological and physical response to food.
 W
WA gastroenterostomy is the surgical creation of a connection between the stomach and the jejunum. The operation can sometimes be performed at the same time as a partial gastrectomy. Gastroenterostomy was in the past typically performed to treat peptic ulcers, but today it is usually carried out to enable food to pass directly to the middle section of the small intestine when it is necessary to bypass the first section because of duodenal damage. The procedure is still being used to treat gastroparesis that is refractory to other treatments, but it is now rarely used to treat peptic ulcers because most cases thereof are bacterial in nature and there are many new drugs available to treat the gastric reflux often experienced with peptic ulcer disease. Reported cure rates for H. pylori infection range from 70% to 90% after antibiotic treatment.
 W
WA proctosigmoidectomy, Hartmann's operation or Hartmann's procedure is the surgical resection of the rectosigmoid colon with closure of the anorectal stump and formation of an end colostomy. It was used to treat colon cancer or inflammation. Currently, its use is limited to emergency surgery when immediate anastomosis is not possible, or more rarely it is used palliatively in patients with colorectal tumours.
 W
WHernia repair refers to a surgical operation for the correction of a hernia—a bulging of internal organs or tissues through the wall that contains it. It can be of two different types: herniorrhaphy; or hernioplasty. This operation may be performed to correct hernias of the abdomen, groin, diaphragm, brain, or at the site of a previous operation. Hernia repair is often performed as an ambulatory procedure.
 W
WIleostomy is a stoma constructed by bringing the end or loop of small intestine out onto the surface of the skin, or the surgical procedure which creates this opening. Intestinal waste passes out of the ileostomy and is collected in an external ostomy system which is placed next to the opening. Ileostomies are usually sited above the groin on the right hand side of the abdomen.
 W
WInguinal hernia surgery is an operation to repair a weakness in the abdominal wall that abnormally allows abdominal contents to slip into a narrow tube called the inguinal canal in the groin region.
 W
WIntestine transplantation is the surgical replacement of the small intestine for chronic and acute cases of intestinal failure. While intestinal failure can oftentimes be treated with alternative therapies such as parenteral nutrition (PN), complications such as PN-associated liver disease and short bowel syndrome may make transplantation the only viable option. One of the rarest type of organ transplantation performed, intestine transplantation is becoming increasingly prevalent as a therapeutic option due to improvements in immunosuppressive regimens, surgical technique, PN, and the clinical management of pre and post-transplant patients.
 W
WJejunostomy is the surgical creation of an opening (stoma) through the skin at the front of the abdomen and the wall of the jejunum. It can be performed either endoscopically, or with open surgery.
 W
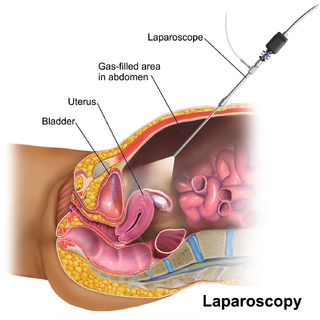
WLaparoscopy is an operation performed in the abdomen or pelvis using small incisions with the aid of a camera. The laparoscope aids diagnosis or therapeutic interventions with a few small cuts in the abdomen.
 W
WNatural orifice transluminal endoscopic surgery (NOTES) is an experimental surgical technique whereby "scarless" abdominal operations can be performed with an endoscope passed through a natural orifice then through an internal incision in the stomach, vagina, bladder or colon, thus avoiding any external incisions or scars.
 W
WA Nissen fundoplication, or laparoscopic Nissen fundoplication when performed via laparoscopic surgery, is a surgical procedure to treat gastroesophageal reflux disease (GERD) and hiatal hernia. In GERD, it is usually performed when medical therapy has failed; but, with a Type II (paraesophageal) hiatus hernia, it is the first-line procedure. The Nissen fundoplication is total (360°), but partial fundoplications known as Thal, Belsey, Dor, Lind, and Toupet fundoplications are alternative procedures with somewhat different indications and outcomes.
 W
WPercutaneous endoscopic gastrostomy (PEG) is an endoscopic medical procedure in which a tube is passed into a patient's stomach through the abdominal wall, most commonly to provide a means of feeding when oral intake is not adequate. This provides enteral nutrition despite bypassing the mouth; enteral nutrition is generally preferable to parenteral nutrition. The PEG procedure is an alternative to open surgical gastrostomy insertion, and does not require a general anesthetic; mild sedation is typically used. PEG tubes may also be extended into the small intestine by passing a jejunal extension tube through the PEG tube and into the jejunum via the pylorus.
 W
WIn general surgery, a Roux-en-Y anastomosis, or Roux-en-Y, is an end-to-side surgical anastomosis of bowel used to reconstruct the gastrointestinal tract. Typically, it is between stomach and small bowel that is distal from the cut end.
 W
WSADI-S is a bariatric surgical technique to lose weight.
 W
WStapled hemorrhoidopexy, is a surgical procedure that involves the removal of abnormally enlarged hemorrhoidal tissue, followed by the repositioning of the remaining hemorrhoidal tissue back to its normal anatomic position. Severe cases of hemorrhoidal prolapse will normally require surgery. Newer surgical procedures include stapled transanal rectal resection (STARR) and procedure for prolapse and hemorrhoids (PPH). Both STARR and PPH are contraindicated in persons with either enterocele or anismus.
 W
WVertical banded gastroplasty (VBG), also known as stomach stapling, is a form of bariatric surgery for weight control. The VBG procedure involves using a band and staples to create a small stomach pouch. In the bottom of the pouch is an approximate one-centimeter hole through which the pouch contents can flow into the remainder of the stomach and hence onto the remainder of the gastrointestinal tract.