 W
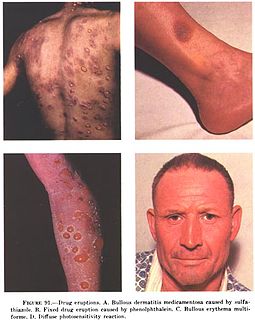
WIn medicine, a drug eruption is an adverse drug reaction of the skin. Most drug-induced cutaneous reactions are mild and disappear when the offending drug is withdrawn. These are called "simple" drug eruptions. However, more serious drug eruptions may be associated with organ injury such as liver or kidney damage and are categorized as "complex". Drugs can also cause hair and nail changes, affect the mucous membranes, or cause itching without outward skin changes.
 W
WAcute generalized exanthematous pustulosis (AGEP) is a rare skin reaction that in 90% of cases is related to medication administration.
 W
WAllopurinol hypersensitivity syndrome typically occurs in persons with preexisting kidney failure. Weeks to months after allopurinol is begun, the patient develops a morbilliform eruption or, less commonly, develops one of the far more serious and potentially lethal severe cutaneous adverse reactions viz., the DRESS syndrome, Stevens Johnson syndrome, or toxic epidermal necrolysis.
 W
WAngioedema is an area of swelling of the lower layer of skin and tissue just under the skin or mucous membranes. The swelling may occur in the face, tongue, larynx, abdomen, or arms and legs. Often it is associated with hives, which are swelling within the upper skin. Onset is typically over minutes to hours.
 W
WMercury poisoning is a type of metal poisoning due to exposure to mercury. Symptoms depend upon the type, dose, method, and duration of exposure. They may include muscle weakness, poor coordination, numbness in the hands and feet, skin rashes, anxiety, memory problems, trouble speaking, trouble hearing, or trouble seeing. High-level exposure to methylmercury is known as Minamata disease. Methylmercury exposure in children may result in acrodynia in which the skin becomes pink and peels. Long-term complications may include kidney problems and decreased intelligence. The effects of long-term low-dose exposure to methylmercury are unclear.
 W
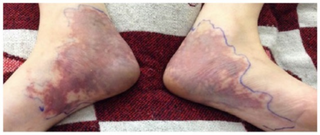
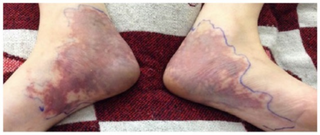
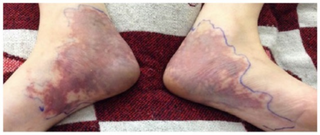
WChemotherapy-induced acral erythema is reddening, swelling, numbness and desquamation on palms of the hands and soles of the feet that can occur after chemotherapy in patients with cancer. Hand-foot syndrome is also rarely seen in sickle-cell disease. These skin changes usually are well demarcated. Acral erythema typically disappears within a few weeks after discontinuation of the offending drug.
 W
WLichen planus (LP) is a chronic inflammatory and immune-mediated disease that affects the skin, nails, hair, and mucous membranes. It is not an actual lichen, and is only named that because it looks like one. It is characterized by polygonal, flat-topped, violaceous papules and plaques with overlying, reticulated, fine white scale, commonly affecting dorsal hands, flexural wrists and forearms, trunk, anterior lower legs and oral mucosa. Although there is a broad clinical range of LP manifestations, the skin and oral cavity remain as the major sites of involvement. The cause is unknown, but it is thought to be the result of an autoimmune process with an unknown initial trigger. There is no cure, but many different medications and procedures have been used in efforts to control the symptoms.
 W
WDrug-induced lupus erythematosus is an autoimmune disorder caused by chronic use of certain drugs. These drugs cause an autoimmune response producing symptoms similar to those of systemic lupus erythematosus (SLE). There are 38 known medications to cause DIL but there are three that report the highest number of cases: hydralazine, procainamide, and quinidine. While the criteria for diagnosing DIL has not been thoroughly established, symptoms of DIL typically present as muscle pain and joint pain. Generally, the symptoms recede after discontinuing use of the drugs.
 W
WLivedoid dermatitis is a iatrogenic cutaneous reaction that occurs immediately after a drug injection. It presents as an immediate, extreme pain around the injection site, with overlying skin rapidly becoming erythematous, violaceous, or blanched and sometimes with reticular pattern. The reaction eventually leads to variable degrees of necrosis to the skin and underlying tissue. The wound eventually heals, but can lead to atrophic, disfiguring scarring.
 W
WErythema multiforme major is a form of rash with skin loss or epidermal detachment.
 W
WErythema multiforme major is a form of rash with skin loss or epidermal detachment.
 W
WMercury poisoning is a type of metal poisoning due to exposure to mercury. Symptoms depend upon the type, dose, method, and duration of exposure. They may include muscle weakness, poor coordination, numbness in the hands and feet, skin rashes, anxiety, memory problems, trouble speaking, trouble hearing, or trouble seeing. High-level exposure to methylmercury is known as Minamata disease. Methylmercury exposure in children may result in acrodynia in which the skin becomes pink and peels. Long-term complications may include kidney problems and decreased intelligence. The effects of long-term low-dose exposure to methylmercury are unclear.
 W
WIododermas are caused by iodides, with the most common sources of exposure being oral and intravenous contrast materials used to treat thyroid disease. The most common type of eruption is an acneiform eruption with numerous acutely inflamed follicular pustules, each surrounded by a ring of hyperemia.
 W
WCutaneous small-vessel vasculitis (CSVV), also known as hypersensitivity vasculitis, cutaneous leukocytoclastic vasculitis, hypersensitivity angiitis, cutaneous leukocytoclastic angiitis, cutaneous necrotizing vasculitis and cutaneous necrotizing venulitis, is inflammation of small blood vessels, characterized by palpable purpura. It is the most common vasculitis seen in clinical practice.
 W
WLichen planus (LP) is a chronic inflammatory and immune-mediated disease that affects the skin, nails, hair, and mucous membranes. It is not an actual lichen, and is only named that because it looks like one. It is characterized by polygonal, flat-topped, violaceous papules and plaques with overlying, reticulated, fine white scale, commonly affecting dorsal hands, flexural wrists and forearms, trunk, anterior lower legs and oral mucosa. Although there is a broad clinical range of LP manifestations, the skin and oral cavity remain as the major sites of involvement. The cause is unknown, but it is thought to be the result of an autoimmune process with an unknown initial trigger. There is no cure, but many different medications and procedures have been used in efforts to control the symptoms.
 W
WLinear IgA bullous dermatosis is a rare immune-mediated blistering skin disease frequently associated with medication exposure, especially vancomycin, with men and women being equally affected. It was first described by Tadeusz Chorzelski in 1979 and may be divided into two types:Adult linear IgA disease is an acquired, autoimmune blistering disease that may present with a clinical pattern of vesicles indistinguishable from dermatitis herpetiformis, or with vesicles and bullae in a bullous pemphigoid-like appearance. This disease can often be difficult to treat even with usually effective medications such as rituximab. Childhood linear IgA disease is an acquired, self-limited bullous disease that may begin by the time the patient is age 2 to 3 and usually remits by age 13.
 W
WLivedoid dermatitis is a iatrogenic cutaneous reaction that occurs immediately after a drug injection. It presents as an immediate, extreme pain around the injection site, with overlying skin rapidly becoming erythematous, violaceous, or blanched and sometimes with reticular pattern. The reaction eventually leads to variable degrees of necrosis to the skin and underlying tissue. The wound eventually heals, but can lead to atrophic, disfiguring scarring.
 W
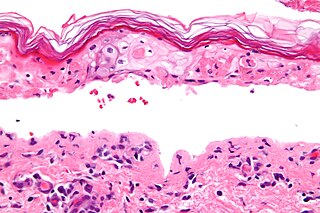
WToxic epidermal necrolysis (TEN) is a type of severe skin reaction. Together with Stevens–Johnson syndrome (SJS) it forms a spectrum of disease, with TEN being more severe. Early symptoms include fever and flu-like symptoms. A few days later the skin begins to blister and peel forming painful raw areas. Mucous membranes, such as the mouth, are also typically involved. Complications include dehydration, sepsis, pneumonia, and multiple organ failure.
 W
WMercury poisoning is a type of metal poisoning due to exposure to mercury. Symptoms depend upon the type, dose, method, and duration of exposure. They may include muscle weakness, poor coordination, numbness in the hands and feet, skin rashes, anxiety, memory problems, trouble speaking, trouble hearing, or trouble seeing. High-level exposure to methylmercury is known as Minamata disease. Methylmercury exposure in children may result in acrodynia in which the skin becomes pink and peels. Long-term complications may include kidney problems and decreased intelligence. The effects of long-term low-dose exposure to methylmercury are unclear.
 W
WLivedoid dermatitis is a iatrogenic cutaneous reaction that occurs immediately after a drug injection. It presents as an immediate, extreme pain around the injection site, with overlying skin rapidly becoming erythematous, violaceous, or blanched and sometimes with reticular pattern. The reaction eventually leads to variable degrees of necrosis to the skin and underlying tissue. The wound eventually heals, but can lead to atrophic, disfiguring scarring.
 W
WChemotherapy-induced acral erythema is reddening, swelling, numbness and desquamation on palms of the hands and soles of the feet that can occur after chemotherapy in patients with cancer. Hand-foot syndrome is also rarely seen in sickle-cell disease. These skin changes usually are well demarcated. Acral erythema typically disappears within a few weeks after discontinuation of the offending drug.
 W
WAcute generalized exanthematous pustulosis (AGEP) is a rare skin reaction that in 90% of cases is related to medication administration.
 W
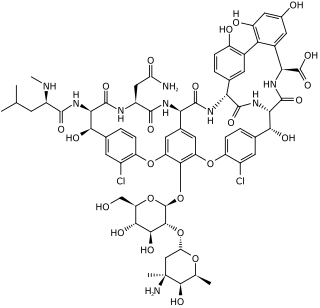
WVancomycin is an antibiotic used to treat a number of bacterial infections. It is recommended intravenously as a treatment for complicated skin infections, bloodstream infections, endocarditis, bone and joint infections, and meningitis caused by methicillin-resistant Staphylococcus aureus. Blood levels may be measured to determine the correct dose. Vancomycin is also recommended by mouth as a treatment for severe Clostridium difficile colitis. When taken by mouth it is very poorly absorbed.
 W
WStevens–Johnson syndrome (SJS) is a type of severe skin reaction. Together with toxic epidermal necrolysis (TEN) and Stevens–Johnson/toxic epidermal necrolysis (SJS/TEN), it forms a spectrum of disease, with SJS being less severe. Erythema multiforme (EM) is generally considered a separate condition. Early symptoms of SJS include fever and flu-like symptoms. A few days later, the skin begins to blister and peel, forming painful raw areas. Mucous membranes, such as the mouth, are also typically involved. Complications include dehydration, sepsis, pneumonia and multiple organ failure.
 W
WToxic epidermal necrolysis (TEN) is a type of severe skin reaction. Together with Stevens–Johnson syndrome (SJS) it forms a spectrum of disease, with TEN being more severe. Early symptoms include fever and flu-like symptoms. A few days later the skin begins to blister and peel forming painful raw areas. Mucous membranes, such as the mouth, are also typically involved. Complications include dehydration, sepsis, pneumonia, and multiple organ failure.
 W
WAcute generalized exanthematous pustulosis (AGEP) is a rare skin reaction that in 90% of cases is related to medication administration.
 W
WWarfarin-induced skin necrosis is a condition in which skin and subcutaneous tissue necrosis occurs due to acquired protein C deficiency following treatment with anti-vitamin K anticoagulants.