 W
WAfterload is the pressure that the heart must work against to eject blood during systole. Afterload is proportional to the average arterial pressure. As aortic and pulmonary pressures increase, the afterload increases on the left and right ventricles respectively. Afterload changes to adapt to the continually changing demands on an animal's cardiovascular system. Afterload is proportional to mean systolic blood pressure and is measured in millimeters of mercury.
 W
WThe ankle-brachial pressure index (ABPI) or ankle-brachial index (ABI) is the ratio of the blood pressure at the ankle to the blood pressure in the upper arm (brachium). Compared to the arm, lower blood pressure in the leg suggests blocked arteries due to peripheral artery disease (PAD). The ABPI is calculated by dividing the systolic blood pressure at the ankle by the systolic blood pressure in the arm.
 W
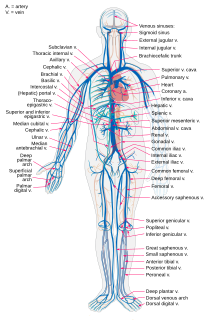
WAn artery is a blood vessel that takes blood away from the heart to one or more parts of the body. Most arteries carry oxygenated blood; the two exceptions are the pulmonary and the umbilical arteries, which carry deoxygenated blood to the organs that oxygenate it. The effective arterial blood volume is that extracellular fluid which fills the arterial system.
 W
WBlood pressure (BP) is the pressure of circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term "blood pressure" refers to the pressure in the large arteries. Blood pressure is usually expressed in terms of the systolic pressure over diastolic pressure in the cardiac cycle. It is measured in millimeters of mercury (mmHg) above the surrounding atmospheric pressure.
 W
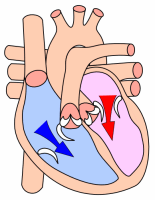
WThe cardiac cycle is the performance of the human heart from the ending of one heartbeat to the beginning of the next. It consists of two periods: one during which the heart muscle relaxes and refills with blood, called diastole, following a period of robust contraction and pumping of blood, dubbed systole. After emptying, the heart immediately relaxes and expands to receive another influx of blood returning from the lungs and other systems of the body, before again contracting to pump blood to the lungs and those systems. A normally performing heart must be fully expanded before it can efficiently pump again. Assuming a healthy heart and a typical rate of 70 to 75 beats per minute, each cardiac cycle, or heartbeat, takes about 0.8 seconds to complete the cycle. There are two atrial and two ventricle chambers of the heart; they are paired as the left heart and the right heart—that is, the left atrium with the left ventricle, the right atrium with the right ventricle—and they work in concert to repeat the cardiac cycle continuously,. At the start of the cycle, during ventricular diastole–early, the heart relaxes and expands while receiving blood into both ventricles through both atria; then, near the end of ventricular diastole–late, the two atria begin to contract, and each atrium pumps blood into the ventricle 'below' it. During ventricular systole the ventricles are contracting and vigorously pulsing two separated blood supplies from the heart—one to the lungs and one to all other body organs and systems—while the two atria are relaxed. This precise coordination ensures that blood is efficiently collected and circulated throughout the body.
 W
WCardiac output (CO), also known as heart output denoted by the symbols , or , is a term used in cardiac physiology that describes the volume of blood being pumped by the heart, by the left and right ventricle, per unit time. Cardiac output (CO) is the product of the heart rate (HR), i.e. the number of heartbeats per minute (bpm), and the stroke volume (SV), which is the volume of blood pumped from the ventricle per beat; thus, CO = HR × SV. Values for cardiac output are usually denoted as L/min. For a healthy person weighing 70 kg, the cardiac output at rest averages about 5 L/min; assuming a heart rate of 70 beats/min, the stroke volume would be approximately 70 ml.
 W
WAn exudate is a fluid emitted by an organism through pores or a wound, a process known as exuding or exudation. Exudate is derived from exude, "to ooze", from the Latin exsūdāre, "to sweat".
 W
WThe Fåhræus effect is the decrease in average concentration of red blood cells in human blood as the diameter of the glass tube in which it is flowing decreases. In other words, in blood vessels with diameters less than 500 micrometers, the hematocrit decreases with decreasing capillary diameter. The Fåhræus effect definitely influences the Fåhræus–Lindqvist effect, which describes the dependence of apparent viscosity of blood on the capillary size, but the former is not the only cause of the latter.
 W
WThe filtered esophageal left heart electrogram is a semi-invasive electrocardiographic method. This technique is able to provide additional information about left atrial and left ventricular activities.
 W
WThe Frank–Starling law of the heart represents the relationship between stroke volume and end diastolic volume. The law states that the stroke volume of the heart increases in response to an increase in the volume of blood in the ventricles, before contraction, when all other factors remain constant. As a larger volume of blood flows into the ventricle, the blood stretches the cardiac muscle fibers, leading to an increase in the force of contraction. The Frank-Starling mechanism allows the cardiac output to be synchronized with the venous return, arterial blood supply and humoral length, without depending upon external regulation to make alterations. The physiological importance of the mechanism lies mainly in maintaining left and right ventricular output equality.
 W
WThe hemodynamics of the aorta is an ongoing field of research in which the goal is to identify what flow patterns and subsequent forces occur within the thoracic aorta. These patterns and forces are used to identify the presence and severity of cardiovascular diseases such as aortic aneurysm and atherosclerosis. Some of the methods used to study the hemodynamics of aortic flow are patient scans, computational fluid dynamics models, and particle tracking velocimetry (PTV). The information gathered through these studies can be used for surgery planning and the development of implants. Greater understanding of this topic reduces mortality rates associated with cardiovascular disease.
 W
WIn cardiac physiology, isovolumetric contraction is an event occurring in early systole during which the ventricles contract with no corresponding volume change (isovolumetrically). This short-lasting portion of the cardiac cycle takes place while all heart valves are closed.
 W
WIsovolumic relaxation time (IVRT) is an interval in the cardiac cycle, from the aortic component of the second heart sound, that is, closure of the aortic valve, to onset of filling by opening of the mitral valve. It can be used as an indicator of diastolic dysfunction.
 W
WThe jugular venous pressure is the indirectly observed pressure over the venous system via visualization of the internal jugular vein. It can be useful in the differentiation of different forms of heart and lung disease. Classically three upward deflections and two downward deflections have been described.The upward deflections are the "a", "c" and "v" = venous filling The downward deflections of the wave are the "x" descent and the "y" descent.
 W
WIn electrocardiography, left axis deviation (LAD) is a condition wherein the mean electrical axis of ventricular contraction of the heart lies in a frontal plane direction between −30° and −90°. This is reflected by a QRS complex positive in lead I and negative in leads aVF and II.
 W
WPerfusion is the passage of fluid through the circulatory system or lymphatic system to an organ or a tissue, usually referring to the delivery of blood to a capillary bed in tissue. Perfusion is measured as the rate at which blood is delivered to tissue, or volume of blood per unit time per unit tissue mass. The SI unit is m3/(s·kg), although for human organs perfusion is typically reported in ml/min/g. The word is derived from the French verb "perfuser" meaning to "pour over or through". All animal tissues require an adequate blood supply for health and life. Poor perfusion (malperfusion), that is, ischemia, causes health problems, as seen in cardiovascular disease, including coronary artery disease, cerebrovascular disease, peripheral artery disease, and many other conditions.
 W
WIn cardiac physiology, preload is the amount of sarcomere stretch experienced by cardiac muscle cells, called cardiomyocytes, at the end of ventricular filling during diastole. Preload is directly related to ventricular filling. As the relaxed ventricle fills during diastole, the walls are stretched and the length of sarcomeres increases. Sarcomere length can be approximated by the volume of the ventricle because each shape has a conserved surface-area-to-volume ratio. This is useful clinically because measuring the sarcomere length is destructive to heart tissue. It requires cutting out a piece of cardiac muscle to look at the sarcomeres under a microscope. It is currently not possible to directly measure preload in the beating heart of a living animal. Preload is estimated from end-diastolic ventricular pressure and is measured in millimeters of mercury (mmHg).
 W
WPressure overload refers to the pathological state of cardiac muscle in which it has to contract while experiencing an excessive afterload. Pressure overload may affect any of the four chambers of the heart, though the term is most commonly applied to one of the two ventricles. Chronic pressure overload leads to concentric hypertrophy of the cardiac muscle, which can in turn lead to heart failure, myocardial ischaemia or, in extreme cases, outflow obstruction.
 W
WA pressure–volume diagram is used to describe corresponding changes in volume and pressure in a system. They are commonly used in thermodynamics, cardiovascular physiology, and respiratory physiology.
 W
WThe renin–angiotensin system (RAS), or renin–angiotensin–aldosterone system (RAAS), is a hormone system that regulates blood pressure and fluid and electrolyte balance, as well as systemic vascular resistance.
 W
WVascular permeability, often in the form of capillary permeability or microvascular permeability, characterizes the capacity of a blood vessel wall to allow for the flow of small molecules or even whole cells in and out of the vessel. Blood vessel walls are lined by a single layer of endothelial cells. The gaps between endothelial cells are strictly regulated depending on the type and physiological state of the tissue.
 W
WVasoconstriction is the narrowing of the blood vessels resulting from contraction of the muscular wall of the vessels, in particular the large arteries and small arterioles. The process is the opposite of vasodilation, the widening of blood vessels. The process is particularly important in controlling hemorrhage and reducing acute blood loss. When blood vessels constrict, the flow of blood is restricted or decreased, thus retaining body heat or increasing vascular resistance. This makes the skin turn paler because less blood reaches the surface, reducing the radiation of heat. On a larger level, vasoconstriction is one mechanism by which the body regulates and maintains mean arterial pressure.
 W
WVasodilation is the widening of blood vessels. It results from relaxation of smooth muscle cells within the vessel walls, in particular in the large veins, large arteries, and smaller arterioles. The process is the opposite of vasoconstriction, which is the narrowing of blood vessels.
 W
WVeins are blood vessels that carry blood towards the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are the pulmonary and umbilical veins, both of which carry oxygenated blood to the heart. In contrast to veins, arteries carry blood away from the heart.
 W
WA ventricle is one of two large chambers toward the bottom of the heart that collect and expel blood received from an atrium towards the peripheral beds within the body and lungs. The atrium primes the pump.
 W
WVolume overload refers to the state of one of the chambers of the heart in which too large a volume of blood exists within it for it to function efficiently. Ventricular volume overload is approximately equivalent to an excessively high preload. It is a cause of cardiac failure.
 W
WA Wiggers diagram, named after its developer, Carl Wiggers, is a standard diagram that is used in teaching cardiac physiology. In the Wiggers diagram, the X-axis is used to plot time, while the Y-axis contains all of the following on a single grid:Blood pressure Aortic pressure Ventricular pressure Atrial pressure Ventricular volume Electrocardiogram Arterial flow (optional) Heart sounds (optional)
 W
WWindkessel effect is a term used in medicine to account for the shape of the arterial blood pressure waveform in terms of the interaction between the stroke volume and the compliance of the aorta and large elastic arteries and the resistance of the smaller arteries and arterioles. Windkessel when loosely translated from German to English means 'air chamber', but is generally taken to imply an elastic reservoir. The walls of large elastic arteries contain elastic fibers, formed of elastin. These arteries distend when the blood pressure rises during systole and recoil when the blood pressure falls during diastole. Since the rate of blood entering these elastic arteries exceeds that leaving them via the peripheral resistance, there is a net storage of blood in the aorta and large arteries during systole, which discharges during diastole. The compliance of the aorta and large elastic arteries is therefore analogous to a capacitor.