 W
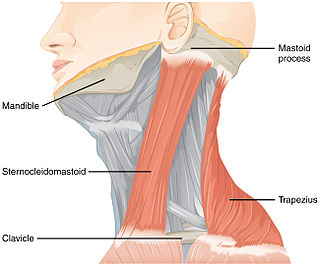
WAccessory nerve disorder is an injury to the spinal accessory nerve which results in diminished or absent function of the sternocleidomastoid muscle and upper portion of the trapezius muscle.
 W
WAlcoholic polyneuropathy is a neurological disorder in which peripheral nerves throughout the body malfunction simultaneously. It is defined by axonal degeneration in neurons of both the sensory and motor systems and initially occurs at the distal ends of the longest axons in the body. This nerve damage causes an individual to experience pain and motor weakness, first in the feet and hands and then progressing centrally. Alcoholic polyneuropathy is caused primarily by chronic alcoholism; however, vitamin deficiencies are also known to contribute to its development. This disease typically occurs in chronic alcoholics who have some sort of nutritional deficiency. Treatment may involve nutritional supplementation, pain management, and abstaining from alcohol.
 W
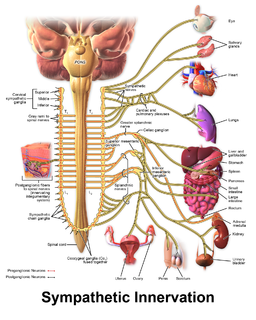
WAutonomic neuropathy is a form of polyneuropathy that affects the non-voluntary, non-sensory nervous system, affecting mostly the internal organs such as the bladder muscles, the cardiovascular system, the digestive tract, and the genital organs. These nerves are not under a person's conscious control and function automatically. Autonomic nerve fibers form large collections in the thorax, abdomen, and pelvis outside the spinal cord. They have connections with the spinal cord and ultimately the brain, however. Most commonly autonomic neuropathy is seen in persons with long-standing diabetes mellitus type 1 and 2. In most—but not all—cases, autonomic neuropathy occurs alongside other forms of neuropathy, such as sensory neuropathy.
 W
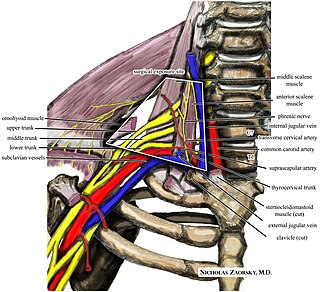
WAxillary nerve dysfunction is any disorder caused by damage to the axillary nerve. The axillary nerve is a branch of the brachial plexus that innervates the deltoid and teres minor muscles. This nerve can be injured or damaged in a variety of ways - penetrating injury such as knife or gunshot wounds, surgical trauma, stretch injury, and various metabolic or rheumatic conditions that may cause focal disruption of the blood supply to the nerve. The exact cause of the axillary nerve dysfunction cannot be identified with electromyography, but the way that the nerve has responded to the injury, and whether or not the nerve is healing, can.
 W
WCharcot–Marie–Tooth disease (CMT) is a hereditary motor and sensory neuropathy of the peripheral nervous system characterized by progressive loss of muscle tissue and touch sensation across various parts of the body. This disease is the most commonly inherited neurological disorder affecting about one in 2,500 people. Currently, there are no curative treatments for this disorder, with care focused on maintaining function. CMT was previously classified as a subtype of muscular dystrophy.
 W
WCongenital insensitivity to pain with anhidrosis (CIPA) is a rare autosomal recessive disorder of the nervous system which prevents the feeling of pain or temperature, and prevents a person from sweating. Cognitive disorders are commonly coincident. CIPA is the fourth type of hereditary sensory and autonomic neuropathy (HSAN), and is also known as HSAN IV.
 W
WDenervation is any loss of nerve supply regardless of the cause. If the nerves lost to denervation are part of the neuronal communication to a specific function in the body then altered or a loss of physiological functioning can occur. Denervation can be caused by injury or be a symptom of a disorder like ALS and post-polio syndrome. Additionally, it can be a useful surgical technique to alleviate major negative symptoms, such as in renal denervation. Denervation can have many harmful side effects such as increased risk of infection and tissue dysfunction.
 W
WDysautonomia or autonomic dysfunction is a condition in which the autonomic nervous system (ANS) does not work properly. This may affect the functioning of the heart, bladder, intestines, sweat glands, pupils, and blood vessels. Dysautonomia has many causes, not all of which may be classified as neuropathic. A number of conditions can feature dysautonomia, such as Parkinson's disease, HIV/AIDS, multiple system atrophy, autonomic failure, postural orthostatic tachycardia syndrome, Ehlers-Danlos syndrome, autoimmune autonomic ganglionopathy, and autonomic neuropathy.
 W
WErythromelalgia, formerly known as Mitchell's disease, is a rare vascular peripheral pain disorder in which blood vessels, usually in the lower extremities or hands, are episodically blocked, then become hyperemic and inflamed. There is severe burning pain and skin redness. The attacks are periodic and are commonly triggered by heat, pressure, mild activity, exertion, insomnia or stress. Erythromelalgia may occur either as a primary or secondary disorder. Secondary erythromelalgia can result from small fiber peripheral neuropathy of any cause, polycythemia vera, essential thrombocytosis, hypercholesterolemia, mushroom or mercury poisoning, and some autoimmune disorders. Primary erythromelalgia is caused by mutation of the voltage-gated sodium channel α-subunit gene SCN9A.
 W
WFacial nerve paralysis is a common problem that involves the paralysis of any structures innervated by the facial nerve. The pathway of the facial nerve is long and relatively convoluted, so there are a number of causes that may result in facial nerve paralysis. The most common is Bell's palsy, a disease of unknown cause that may only be diagnosed by exclusion of identifiable serious causes.
 W
WHorner's syndrome, also known as oculosympathetic paresis, is a combination of symptoms that arises when a group of nerves known as the sympathetic trunk is damaged. The signs and symptoms occur on the same side (ipsilateral) as it is a lesion of the sympathetic trunk. It is characterized by miosis, partial ptosis, apparent anhydrosis, with apparent enophthalmos.
 W
WMultiple system atrophy (MSA) is a rare neurodegenerative disorder characterized by autonomic dysfunction, tremors, slow movement, muscle rigidity, and postural instability and ataxia. This is caused by progressive degeneration of neurons in several parts of the brain including the basal ganglia, inferior olivary nucleus, and cerebellum.
 W
WNerve compression syndrome or compression neuropathy, is a medical condition caused by direct pressure on a nerve. It is known colloquially as a trapped nerve, though this may also refer to nerve root compression. Its symptoms include pain, tingling, numbness and muscle weakness. The symptoms affect just one particular part of the body, depending on which nerve is affected. Nerve conduction studies help to confirm the diagnosis. In some cases, surgery may help to relieve the pressure on the nerve but this does not always relieve all the symptoms. Nerve injury by a single episode of physical trauma is in one sense a compression neuropathy but is not usually included under this heading.
 W
WNerve injury is injury to nervous tissue. There is no single classification system that can describe all the many variations of nerve injury. In 1941, Seddon introduced a classification of nerve injuries based on three main types of nerve fiber injury and whether there is continuity of the nerve. Usually, however, (peripheral) nerve injury is classified in five stages, based on the extent of damage to both the nerve and the surrounding connective tissue, since supporting glial cells may be involved. Unlike in the central nervous system, neuroregeneration in the peripheral nervous system is possible. The processes that occur in peripheral regeneration can be divided into the following major events: Wallerian degeneration, axon regeneration/growth, and nerve reinnervation. The events that occur in peripheral regeneration occur with respect to the axis of the nerve injury. The proximal stump refers to the end of the injured neuron that is still attached to the neuron cell body; it is the part that regenerates. The distal stump refers to the end of the injured neuron that is still attached to the end of the axon; it is the part of the neuron that will degenerate but that remains in the area toward which the regenerating axon grows. The study of peripheral nerve injury began during the American Civil War and has greatly expanded to the point of using growth-promoting molecules.
 W
WNeuritis is inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation, and frequently concomitant demyelination, cause impaired conduction of neural signals and leads to aberrant nerve function. Neuritis is often conflated with neuropathy, a broad term describing any disease process which affects the peripheral nervous system. However, neuropathies may be due to either inflammatory or non-inflammatory causes, and the term encompasses any form of damage, degeneration, or dysfunction, while neuritis refers specifically to the inflammatory process.
 W
WPeripheral neuropathy, often shortened to neuropathy, is a general term describing disease affecting the peripheral nerves, meaning nerves beyond the brain and spinal cord. Damage to peripheral nerves may impair sensation, movement, gland or organ function depending on which nerves are affected; in other words, neuropathy affecting motor, sensory, or autonomic nerves result in different symptoms. More than one type of nerve may be affected simultaneously. Peripheral neuropathy may be acute or chronic, and may be reversible or permanent.
 W
WPiriformis syndrome is a condition which is believed to result from compression of the sciatic nerve by the piriformis muscle. Symptoms may include pain and numbness in the buttocks and down the leg. Often symptoms are worsened with sitting or running.
 W
WPolyneuropathy is damage or disease affecting peripheral nerves in roughly the same areas on both sides of the body, featuring weakness, numbness, and burning pain. It usually begins in the hands and feet and may progress to the arms and legs and sometimes to other parts of the body where it may affect the autonomic nervous system. It may be acute or chronic. A number of different disorders may cause polyneuropathy, including diabetes and some types of Guillain–Barré syndrome.
 W
WPostural orthostatic tachycardia syndrome (POTS) is a condition in which a change from lying to standing causes an abnormally large increase in heart rate. This occurs with symptoms that may include lightheadedness, trouble thinking, blurred vision or weakness. Other commonly associated conditions include Ehlers–Danlos syndrome, mast cell activation syndrome, irritable bowel syndrome, insomnia, chronic headaches, chronic fatigue syndrome and fibromyalgia.
 W
WPronator teres syndrome is a compression neuropathy of the median nerve at the elbow. It is rare compared to compression at the wrist or isolated injury of the anterior interosseous branch of the median nerve.
 W
WQuadrilateral space syndrome is a rotator cuff denervation syndrome in which the axillary nerve is compressed at the quadrilateral space of the rotator cuff.
 W
WRadial nerve dysfunction is a problem associated with the radial nerve resulting from injury consisting of acute trauma to the radial nerve. The damage has sensory consequences, as it interferes with the radial nerve's innervation of the skin of the posterior forearm, lateral three digits, and the dorsal surface of the lateral side of the palm. The damage also has motor consequences, as it interferes with the radial nerve's innervation of the muscles associated with the extension at the elbow, wrist, and fingers, as well the supination of the forearm. This type of injury can be difficult to localize, but relatively common, as many ordinary occurrences can lead to the injury and resulting mononeuropathy. One out of every ten patients suffering from radial nerve dysfunction do so because of a fractured humerus.
 W
WRadial neuropathy is a type of mononeuropathy which results from acute trauma to the radial nerve that extends the length of the arm. It is known as transient paresthesia when sensation is temporarily abnormal.
 W
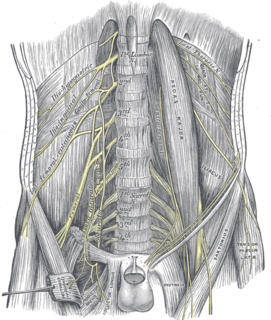
WRadiation-induced lumbar plexopathy (RILP) or radiation-induced lumbosacral plexopathy (RILSP) is nerve damage in the pelvis and lower spine area caused by therapeutic radiation treatments. RILP is a rare side effect of external beam radiation therapy and both interstitial and intracavity brachytherapy radiation implants.
 W
WRadiculopathy, also commonly referred to as pinched nerve, refers to a set of conditions in which one or more nerves are affected and do not work properly. This can result in pain, weakness, numbness, or difficulty controlling specific muscles.
 W
WSciatica is pain going down the leg from the lower back. This pain may go down the back, outside, or front of the leg. Onset is often sudden following activities like heavy lifting, though gradual onset may also occur. The pain is often described as shooting. Typically, symptoms are only on one side of the body. Certain causes, however, may result in pain on both sides. Lower back pain is sometimes present. Weakness or numbness may occur in various parts of the affected leg and foot.
 W
WThoracic outlet syndrome (TOS) is a condition in which there is compression of the nerves, arteries, or veins in the passageway from the lower neck to the armpit. There are three main types: neurogenic, venous, and arterial. The neurogenic type is the most common and presents with pain, weakness, and occasionally loss of muscle at the base of the thumb. The venous type results in swelling, pain, and possibly a bluish coloration of the arm. The arterial type results in pain, coldness, and paleness of the arm.
 W
WUlnar neuropathy is a disorder involving the ulnar nerve. Ulnar neuropathy may be caused by entrapment of the ulnar nerve with resultant numbness and tingling. Motor function can be assessed by testing for a positive Froment's sign, or making an OK sign, little finger abduction can be tested as well.
 W
WA winged scapula is a skeletal medical condition in which the shoulder blade protrudes from a person's back in an abnormal position.