 W
WCardiac electrophysiology is the science of elucidating, diagnosing, and treating the electrical activities of the heart. The term is usually used in a clinical context to describe studies of such phenomena by invasive (intracardiac) catheter recording of spontaneous activity as well as of cardiac responses to programmed electrical stimulation (PES), see Clinical cardiac electrophysiology. Cardiac electrophysiology also encompasses basic research and translational research components. Someone who studies cardiac electrophysiology, either clinically or solely through research, is known as a cardiac electrophysiologist.
 W
WAntiarrhythmic agents, also known as cardiac dysrhythmia medications, are a group of pharmaceuticals that are used to suppress abnormal rhythms of the heart, such as atrial fibrillation, atrial flutter, ventricular tachycardia, and ventricular fibrillation.
 W
WA cardiac pacemaker, is a medical device that generates electrical impulses delivered by electrodes to cause the heart muscle chambers to contract and therefore pump blood; by doing so this device replaces and/or regulates the function of the electrical conduction system of the heart.
 W
WAsian Heart Institute (AHI), is a cardiac care hospital, established in 2002, located in the western suburb of Bandra, at the Bandra-Kurla Complex (BKC), in Mumbai, Maharashtra, India. It has pioneered the treatment of complex heart surgeries, arterial graft & beating heart surgery in India.
 W
WAn automated external defibrillator (AED) is a portable electronic device that automatically diagnoses the life-threatening cardiac arrhythmias of ventricular fibrillation (VF) and pulseless ventricular tachycardia, and is able to treat them through defibrillation, the application of electricity which stops the arrhythmia, allowing the heart to re-establish an effective rhythm.
 W
WA bundle branch block is a defect of the bundle branches or fascicles in the electrical conduction system of the heart.
 W
WDiscovered in 1893 by Swiss-born cardiologist and anatomist Wilhelm His Jr., the bundle of His (BH) or His bundle (HB) ( "hiss") is a collection of heart muscle cells specialized for electrical conduction. As part of the electrical conduction system of the heart, it transmits the electrical impulses from the AV node to the point of the apex of the fascicular branches via the bundle branches. The fascicular branches then lead to the Purkinje fibers, which provide electrical conduction to the ventricles, causing the cardiac muscle of the ventricles to contract at a paced interval.
 W
WClassical cable theory uses mathematical models to calculate the electric current along passive neurites, particularly the dendrites that receive synaptic inputs at different sites and times. Estimates are made by modeling dendrites and axons as cylinders composed of segments with capacitances and resistances combined in parallel. The capacitance of a neuronal fiber comes about because electrostatic forces are acting through the very thin lipid bilayer. The resistance in series along the fiber is due to the axoplasm's significant resistance to movement of electric charge.
 W
WCardiac monitoring generally refers to continuous or intermittent monitoring of heart activity, generally by electrocardiography, with assessment of the patient's condition relative to their cardiac rhythm. It is different from hemodynamic monitoring, which monitors the pressure and flow of blood within the cardiovascular system. The two may be performed simultaneously on critical heart patients. Cardiac monitoring with a small device worn by an ambulatory patient is known as ambulatory electrocardiography. Transmitting data from a monitor to a distant monitoring station is known as telemetry or biotelemetry.
 W
WCardiac muscle is one of three types of vertebrate muscles, with the other two being skeletal and smooth muscles. It is an involuntary, striated muscle that constitutes the main tissue of the walls of the heart. The myocardium forms a thick middle layer between the outer layer of the heart wall and the inner layer, with blood supplied via the coronary circulation. It is composed of individual heart muscle cells (cardiomyocytes) joined together by intercalated discs, encased by collagen fibers and other substances that form the extracellular matrix.
 W
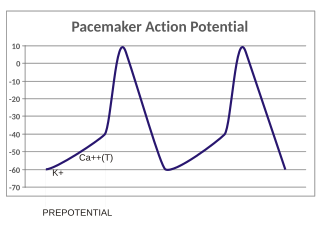
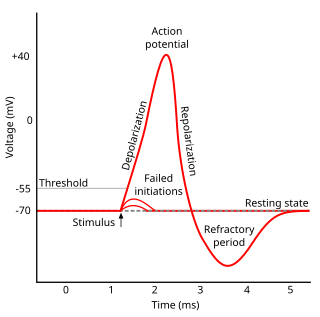
WThe contraction of cardiac muscle in all animals is initiated by electrical impulses known as action potentials. The rate at which these impulses fire, controls the rate of cardiac contraction, that is, the heart rate. The cells that create these rhythmic impulses, setting the pace for blood pumping, are called pacemaker cells, and they directly control the heart rate. They make up the cardiac pacemaker, that is, the natural pacemaker of the heart. In most humans, the concentration of pacemaker cells in the sinoatrial (SA) node is the natural pacemaker, and the resultant rhythm is a sinus rhythm.
 W
WCardiac Pacemakers, Inc.(CPI), doing business as Guidant Cardiac Rhythm Management, manufactured implantable cardiac rhythm management devices, such as pacemakers and defibrillators. It also sold insulin pumps controlled by microprocessors and various equipments to regulate heart rhythm. In addition, Cardiac Pacemakers, Inc. developed therapies for the treatment of irregular heartbeats. The company was founded in 1971 and is based in St. Paul, Minnesota. Cardiac Pacemakers, Inc. operates as a subsidiary of Boston Scientific Corporation.
 W
WCardiac resynchronisation therapy is the insertion of electrodes in the left and right ventricles of the heart, as well as on occasion the right atrium, to treat heart failure by coordinating the function of the left and right ventricles via a pacemaker, a small device inserted into the interior chest wall.
 W
WThe cardiac transient outward potassium current (referred to as Ito1 or Ito ) is one of the ion currents across the cell membrane of heart muscle cells. It is the main contributing current during the repolarizing phase 1 of the cardiac action potential. It is a result of the movement of positively charged potassium (K+) ions from the intracellular to the extracellular space. Ito1 is complemented with Ito2 resulting from Cl− ions to form the transient outward current Ito.
 W
WConcealed conduction is tissue stimulation without direct effect, but leading to a change in conduction characteristics.
 W
WRoss Cowie is a charity-worker and former shinty player and manager, from Portree, Isle of Skye, Scotland. He is affectionately known as The Colonel.
 W
WDefibrillation is a treatment for life-threatening cardiac dysrhythmias, specifically ventricular fibrillation (VF) and non-perfusing ventricular tachycardia (VT). A defibrillator delivers a dose of electric current to the heart. Although not fully understood, this process depolarizes a large amount of the heart muscle, ending the dysrhythmia. Subsequently, the body's natural pacemaker in the sinoatrial node of the heart is able to re-establish normal sinus rhythm. A heart which is in asystole (flatline) cannot be restarted by a defibrillator, but would be treated by cardiopulmonary resuscitation (CPR).
 W
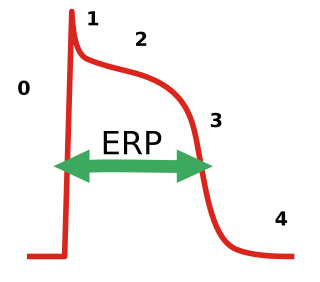
WIn electrocardiography, during a cardiac cycle, once an action potential is initiated, there is a period of time that a new action potential cannot be initiated. This is termed the effective refractory period (ERP) of the tissue. This period is approximately equal to the absolute refractory period (ARP), it occurs because the fast sodium channels remain closed until the cell fully repolarizes. During this period, depolarization on adjacent cardiac muscles does not produce a new depolarization in the current cell as it has to refract back to phase 4 of the action potential before a new action potential can activate it. ERP acts as a protective mechanism and keeps the heart rate in check and prevents arrhythmias, and it helps coordinates muscle contraction. Anti-arrhythmic agents used for arrhythmias usually prolong the ERP. For the treatment of atrial fibrillation, it is a problem that the prolongation of the ERP by these agents also affects the ventricles, which can induce other types of arrhythmias.
 W
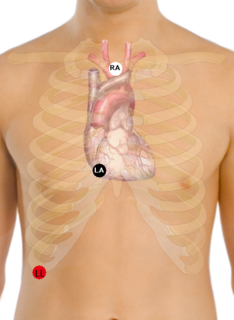
WEinthoven's triangle is an imaginary formation of three limb leads in a triangle used in electrocardiography, formed by the two shoulders and the pubis. The shape forms an inverted equilateral triangle with the heart at the center. It is named after Willem Einthoven, who theorized its existence.
 W
WThe electrical conduction system of the heart transmits signals generated usually by the sinoatrial node to cause contraction of the heart muscle. The pacemaking signal generated in the sinoatrial node travels through the right atrium to the atrioventricular node, along the Bundle of His and through bundle branches to cause contraction of the heart muscle. This signal stimulates contraction first of the right and left atrium, and then the right and left ventricles. This process allows blood to be pumped throughout the body.
 W
WElectrocardiography is the process of producing an electrocardiogram. It is a graph of voltage versus time of the electrical activity of the heart using electrodes placed on the skin. These electrodes detect the small electrical changes that are a consequence of cardiac muscle depolarization followed by repolarization during each cardiac cycle (heartbeat). Changes in the normal ECG pattern occur in numerous cardiac abnormalities, including cardiac rhythm disturbances, inadequate coronary artery blood flow, and electrolyte disturbances.
 W
WElectrocardiography in suspected myocardial infarction has the main purpose of detecting ischemia or acute coronary injury in emergency department populations coming for symptoms of myocardial infarction (MI). Also, it can distinguish clinically different types of myocardial infarction.
 W
WThe forward problem of electrocardiology is a computational and mathematical approach to study the electrical activity of the heart through the body surface. The principal aim of this study is to computationally reproduce an electrocardiogram (ECG), which has important clinical relevance to define cardiac pathologies such as ischemia and infarction, or to test pharmaceutical intervention. Given their important functionalities and the relative small invasiveness, the electrocardiography techniques are used quite often as clinical diagnostic tests. Thus, it is natural to proceed to computationally reproduce an ECG, which means to mathematically model the cardiac behaviour inside the body.
 W
WAn implantable cardioverter-defibrillator (ICD) or automated implantable cardioverter defibrillator (AICD) is a device implantable inside the body, able to perform cardioversion, defibrillation, and pacing of the heart. The device is therefore capable of correcting most life-threatening cardiac arrhythmias. The ICD is the first-line treatment and prophylactic therapy for patients at risk for sudden cardiac death due to ventricular fibrillation and ventricular tachycardia. Current devices can be programmed to detect abnormal heart rhythms and deliver therapy via programmable antitachycardia pacing in addition to low-energy and high-energy shocks.
 W
WKv7.1 (KvLQT1) is a potassium channel protein whose primary subunit in humans is encoded by the KCNQ1 gene. Kv7.1 is a voltage and lipid-gated potassium channel present in the cell membranes of cardiac tissue and in inner ear neurons among other tissues. In the cardiac cells, Kv7.1 mediates the IKs (or slow delayed rectifying K+) current that contributes to the repolarization of the cell, terminating the cardiac action potential and thereby the heart's contraction. It is a member of the KCNQ family of potassium channels.
 W
WA Lewis Lead is a modified ECG lead used to detect atrial flutter waves when atrial flutter is suspected clinically, based on signs and symptoms, but is not definitely demonstrated on the standard 12 lead ECG. In order to create the Lewis Lead, the right arm electrode is moved to the manubrium adjacent to the sternum. Then the left arm electrode is moved to the right, fifth intercostal space adjacent to the sternum. The left leg electrode is placed on the right lower costal margin. The Lewis Lead is then read as Lead I on the ECG and, since in most patients it will be roughly perpendicular to the wave of ventricular depolarization, atrial flutter waves may be more apparent.
 W
WThe Libin Cardiovascular Institute of Alberta is a partnership between Alberta Health Services and the University of Calgary. Its mandate comprises all cardiovascular research, education and service delivery, with a service area extending from Saskatchewan, Southern Alberta and Eastern British Columbia. The Institute coordinates the activities of 1,500 individuals in Southern Alberta. Of its more than 175 research and clinician members, over 65 are cardiologists, making it the largest heart or cardiovascular institute in Western Canada by that measure.
 W
WLIFE PAK is a series of vital signs monitors and external cardiac defibrillators produced by medical technology company Physio Control.
 W
WThe P wave on the ECG represents atrial depolarization, which results in atrial contraction, or atrial systole.
 W
WIn the pacemaking cells of the heart (e.g., the sinoatrial node), the pacemaker potential (also called the pacemaker current) is the slow, positive increase in voltage across the cell's membrane (the membrane potential) that occurs between the end of one action potential and the beginning of the next action potential. This increase in membrane potential is what causes the cell membrane, which typically maintains a resting membrane potential of -70 mV, to reach the threshold potential and consequently fire the next action potential; thus, the pacemaker potential is what drives the self-generated rhythmic firing (automaticity) of pacemaker cells, and the rate of change (i.e., the slope) of the pacemaker potential is what determines the timing of the next action potential and thus the intrinsic firing rate of the cell. In a healthy sinoatrial node (SAN, a complex tissue within the right atrium containing pacemaker cells that normally determine the intrinsic firing rate for the entire heart), the pacemaker potential is the main determinant of the heart rate. Because the pacemaker potential represents the non-contracting time between heart beats (diastole), it is also called the diastolic depolarization. The amount of net inward current required to move the cell membrane potential during the pacemaker phase is extremely small, in the order of few pAs, but this net flux arises from time to time changing contribution of several currents that flow with different voltage and time dependence. Evidence in support of the active presence of K+, Ca2+, Na+ channels and Na+/K+ exchanger during the pacemaker phase have been variously reported in the literature, but several indications point to the “funny”(If) current as one of the most important.(see funny current). There is now substantial evidence that also sarcoplasmic reticulum (SR) Ca2+-transients participate to the generation of the diastolic depolarization via a process involving the Na–Ca exchanger.
 W
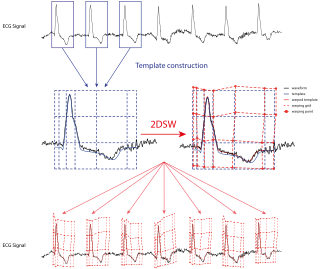
WThe Pan–Tompkins algorithm is commonly used to detect QRS complexes in electrocardiographic signals (ECG). The QRS complex represents the ventricular depolarization and the main spike visible in an ECG signal. This feature makes it particularly suitable for measuring heart rate, the first way to assess the heart health state. In the first derivation of Einthoven of a physiological heart, the QRS complex is composed by a downward deflection, a high upward deflection and a final downward deflection.
 W
WIn electrocardiography, the PR interval is the period, measured in milliseconds, that extends from the beginning of the P wave until the beginning of the QRS complex ; it is normally between 120 and 200 ms in duration. The PR interval is sometimes termed the PQ interval.
 W
WThe Purkinje fibers are located in the inner ventricular walls of the heart, just beneath the endocardium in a space called the subendocardium. The Purkinje fibers are specialised conducting fibers composed of electrically excitable cells. They are larger than cardiomyocytes with fewer myofibrils and many mitochondria. They conduct cardiac action potentials more quickly and efficiently than any other cells in the heart. Purkinje fibers allow the heart's conduction system to create synchronized contractions of its ventricles, and are essential for maintaining a consistent heart rhythm.
 W
WThe QRS complex is the combination of three of the graphical deflections seen on a typical electrocardiogram. It is usually the central and most visually obvious part of the tracing; in other words, it's the main spike seen on an ECG line. It corresponds to the depolarization of the right and left ventricles of the human heart and contraction of the large ventricular muscles.
 W
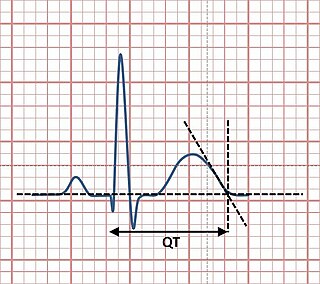
WThe QT interval is a measurement made on an electrocardiogram used to assess some of the electrical properties of the heart. It is calculated as the time from the start of the Q wave to the end of the T wave, and approximates to the time taken from when the cardiac ventricles start to contract to when they finish relaxing. An abnormally long or abnormally short QT interval is associated with an increased risk of developing abnormal heart rhythms and sudden cardiac death. Abnormalities in the QT interval can be caused by genetic conditions such as long QT syndrome, by certain medications such as sotalol or pitolisant, by disturbances in the concentrations of certain salts within the blood such as hypokalaemia, or by hormonal imbalances such as hypothyroidism.
 W
WQT interval variability (QTV) refers to the physiological phenomenon of beat-to-beat fluctuations in QT interval of electrocardiograms. Increased QTV appears to be a marker of arrhythmic and cardiovascular death; it may also play a role for noninvasive assessment of sympathetic nervous system activity.
 W
WRefractoriness is the fundamental property of any object of autowave nature not to respond on stimuli, if the object stays in the specific refractory state. In common sense, refractory period is the characteristic recovery time, a period that is associated with the motion of the image point on the left branch of the isocline .
 W
WSinoventricular conduction is a rare form of cardiac conduction in which the sinoatrial node generates an impulse that is conducted to the atrioventricular node in the absence of the right atrium contracting. This is the physiological proof for the presence of the internodal tracts, which have not been clearly demonstrated histologically. On electrocardiogram (ECG), there will be no P wave due to the inactivation of the atrial muscles.
 W
WIn electrocardiography, the ST segment connects the QRS complex and the T wave and has a duration of 0.005 to 0.150 sec.
 W
WIn electrocardiography, the T wave represents the repolarization of the ventricles. The interval from the beginning of the QRS complex to the apex of the T wave is referred to as the absolute refractory period. The last half of the T wave is referred to as the relative refractory period or vulnerable period. The T wave contains more information than the QT interval. The T wave can be described by its symmetry, skewness, slope of ascending and descending limbs, amplitude and subintervals like the Tpeak–Tend interval.
 W
WTranscutaneous pacing is a temporary means of pacing a patient's heart during a medical emergency. It should not be confused with defibrillation using a manual or automatic defibrillator, though some newer defibrillators can do both, and pads and an electrical stimulus to the heart are used in transcutaneous pacing and defibrillation. Transcutaneous pacing is accomplished by delivering pulses of electric current through the patient's chest, which stimulates the heart to contract.
 W
WThe 'U' wave is a wave on an electrocardiogram (ECG). It comes after the T wave of ventricular repolarization and may not always be observed as a result of its small size. 'U' waves are thought to represent repolarization of the Purkinje fibers. However, the exact source of the U wave remains unclear. The most common theories for the origin are:Delayed repolarization of Purkinje fibers Prolonged re-polarisation of mid-myocardial M-cells After-potentials resulting from mechanical forces in the ventricular wall The repolarization of the papillary muscle.
 W
WIn electrocardiography, the ventricular cardiomyocyte membrane potential is about −90 mV at rest, which is close to the potassium reversal potential. When an action potential is generated, the membrane potential rises above this level in four distinct phases.