 W
WA respiratory therapist is a specialized healthcare practitioner trained in critical care and cardio-pulmonary medicine in order to work therapeutically with people suffering from acute critical conditions, cardiac and pulmonary disease. Respiratory therapists graduate from a college or university with a degree in respiratory therapy and have passed a national board certifying examination. The NBRC is the not-for-profit organization responsible for credentialing the seven areas of Respiratory Therapy in the United States.
 W
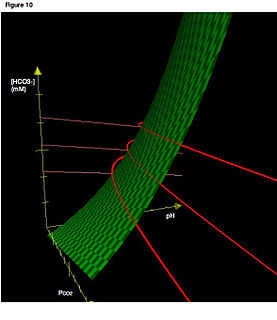
WAcid–base imbalance is an abnormality of the human body's normal balance of acids and bases that causes the plasma pH to deviate out of the normal range. In the fetus, the normal range differs based on which umbilical vessel is sampled. It can exist in varying levels of severity, some life-threatening.
 W
WThe general term nebulizer refers to an apparatus that converts liquids into a fine mist. Nozzles also convert liquids into a fine mist, but do so by pressure through small holes. Nebulizers generally use gas flows to deliver the mist. The most common form of nebulizers are medical appliances such as asthma inhalers or paint spray cans. Analytical nebulizers are a special category in that their purpose is to deliver a fine mist to spectrometric instruments for elemental analysis. They are necessary parts of inductively coupled plasma atomic emission spectroscopy (ICP-AES), inductively coupled plasma mass spectrometry (ICP-MS), and atomic absorption spectroscopy (AAS).
 W
WAn arterial-blood gas (ABG) test measures the amounts of arterial gases, such as oxygen and carbon dioxide. An ABG test requires that a small volume of blood be drawn from the radial artery with a syringe and a thin needle, but sometimes the femoral artery in the groin or another site is used. The blood can also be drawn from an arterial catheter.
 W
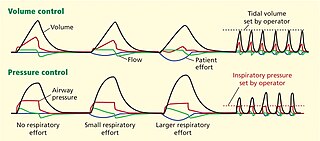
WArtificial ventilation is a means of assisting or stimulating respiration, a metabolic process referring to the overall exchange of gases in the body by pulmonary ventilation, external respiration, and internal respiration. It may take the form of manually providing air for a person who is not breathing or is not making sufficient respiratory effort, or it may be mechanical ventilation involving the use of a mechanical ventilator to move air in and out of the lungs when an individual is unable to breathe on their own, for example during surgery with general anesthesia or when an individual is in a coma or trauma.
 W
WAsthma is a long-term inflammatory disease of the airways of the lungs. It is characterized by variable and recurring symptoms, reversible airflow obstruction, and easily triggered bronchospasms. Symptoms include episodes of wheezing, coughing, chest tightness, and shortness of breath. These may occur a few times a day or a few times per week. Depending on the person, asthma symptoms may become worse at night or with exercise.
 W
WAtelectasis is the collapse or closure of a lung resulting in reduced or absent gas exchange. It is usually unilateral, affecting part or all of one lung. It is a condition where the alveoli are deflated down to little or no volume, as distinct from pulmonary consolidation, in which they are filled with liquid. It is often called a collapsed lung, although that term may also refer to pneumothorax.
 W
WAtelectotrauma, atelectrauma, cyclic atelectasis or repeated alveolar collapse and expansion (RACE) are medical terms for the damage caused to the lung by mechanical ventilation under certain conditions. When parts of the lung collapse at the end of expiration, due to a combination of a diseased lung state and a low functional residual capacity, then reopen again on inspiration, this repeated collapsing and reopening causes shear stress which has a damaging effect on the alveolus. Clinicians attempt to reduce atelectotrauma by ensuring adequate positive end-expiratory pressure (PEEP) to maintain the alveoli open in expiration. This is known as open lung ventilation. High frequency oscillatory ventilation (HFOV) with its use of 'super CPAP' is especially effective in preventing atelectotrauma since it maintains a very high mean airway pressure (MAP), equivalent to a very high PEEP. Atelectotrauma is one of several means by which mechanical ventilation may damage the lungs leading to ventilator-associated lung injury. The other means are volutrauma, barotrauma, rheotrauma and biotrauma. Attempts have been made to combine these factors in an all encompassing term: mechanical power.
 W
WThe Both respirator, also known as the Both Portable Cabinet Respirator, was a negative pressure ventilator invented by Edward Both in 1937. Made from plywood, the respirator was an affordable alternative to the more expensive designs that had been used prior to its development, and accordingly came into common usage in Australia. More widespread use emerged during the 1940s and 1950s, when the Both respirator was offered free of charge to Commonwealth hospitals by William Morris.
 W
WBrittle asthma is a type of asthma distinguishable from other forms by recurrent, severe attacks. There are two subtypes divided by symptoms: Type 1 and Type 2, depending on the stability of the patient's maximum speed of expiration, or peak expiratory flow rate (PEFR). Type 1 is characterized by sustained, chronic variability of PEFR, while type 2 is distinguished by sudden unpredictable drops in PEFR where asthma symptoms are otherwise well controlled and the function of the lungs is not substantially impaired.
 W
WDual-control modes of ventilation are auto-regulated pressure-controlled modes of mechanical ventilation with a user-selected tidal volume target. The ventilator adjusts the pressure limit of the next breath as necessary according to the previous breath's measured exhaled tidal volume. Peak airway pressure varies from breath to breath according to changes in the patient's airway resistance and lung compliance.
 W
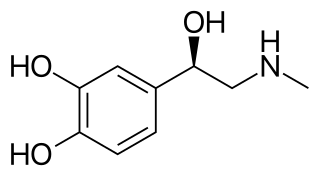
WEpinephrine, also known as adrenaline, is a medication and hormone. As a medication, it is used to treat a number of conditions, including anaphylaxis, cardiac arrest, asthma, and superficial bleeding. Inhaled epinephrine may be used to improve the symptoms of croup. It may also be used for asthma when other treatments are not effective. It is given intravenously, by injection into a muscle, by inhalation, or by injection just under the skin.
 W
WIn medicine, exhaled nitric oxide (eNO) can be measured in a breath test for asthma or other conditions characterized by airway inflammation. Nitric oxide (NO) is a gaseous molecule produced by certain cell types in an inflammatory response. The fraction of exhaled NO (FENO) is a promising biomarker for the diagnosis, follow-up and as a guide to therapy in adults and children with asthma. The breath test has recently become available in many well-equipped hospitals in developed countries, although its exact role remains unclear.
 W
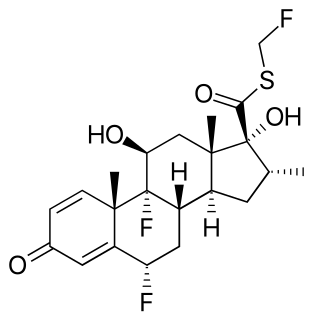
WFluticasone are two manufactured steroids used to treat nasal symptoms. Both the esters, fluticasone furoate and fluticasone propionate, are also used as topical anti-inflammatories and inhaled corticosteroids, and are used much more commonly in comparison.
 W
WFluticasone propionate, sold under the brand names Flovent and Flonase among others, is a steroid medication. When inhaled it is used for the long term management of asthma and COPD. In the nose it is used for hay fever and nasal polyps. It can also be used for mouth ulcers.
 W
WHeated humidified high-flow (HHHF) therapy, often also high flow nasal cannula(e) (HFNC) or high flow nasal oxygen (HFNO), is a type of respiratory support method that delivers a high flow of medical gas to a patient through an interface intended to create a wash-out of the upper airway. The applied gas is heated to best match human body temperature (37 °C) and humidified targeting ideal body saturation vapor pressure. It is used in acute and chronic breathing problems, and is a suitable choice for treatment of patients with severe or critical COVID-19.
 W
WHyperbaric medicine is medical treatment in which an ambient pressure greater than sea level atmospheric pressure is a necessary component. The treatment comprises hyperbaric oxygen therapy (HBOT), the medical use of oxygen at an ambient pressure higher than atmospheric pressure, and therapeutic recompression for decompression illness, intended to reduce the injurious effects of systemic gas bubbles by physically reducing their size and providing improved conditions for elimination of bubbles and excess dissolved gas.
 W
WHyperbaric treatment schedules or hyperbaric treatment tables, are planned sequences of events in chronological order for hyperbaric pressure exposures specifying the pressure profile over time and the breathing gas to be used during specified periods, for medical treatment. Hyperbaric therapy is based on exposure to pressures greater than normal atmospheric pressure, and in many cases the use of breathing gases with oxygen content greater than that of air.
 W
WAn incentive spirometer is a medical device used to help patients improve the functioning of their lungs. It is a simplified spirometer provided to patients who have had any surgery that might jeopardize respiratory function, particularly surgery to the lungs, but also commonly to patients recovering from cardiac or other surgery involving extended time under anesthesia and prolonged in-bed recovery. The incentive spirometer also is issued to patients recovering from pneumonia or rib damage to help minimize the chance of fluid build-up in the lungs. It may be used as well by wind instrument players, who want to improve their air flow.
 W
WAn inhaler is a medical device used for delivering medicines into the lungs through the work of a person's breathing. This allows medicines to be delivered to and absorbed in the lungs, which provides the ability for targeted medical treatment to this specific region of the body, as well as a reduction in the side effects of oral medications. There are a wide variety of inhalers, and they are commonly used to treat numerous medical conditions with asthma and chronic obstructive pulmonary disease (COPD) being among the most notable.
 W
WThe Irish Thoracic Society (ITS) is the official society for professionals involved in the care of people with chronic or acute respiratory disease in Ireland. Membership of the Society is drawn from respiratory physicians, internal medicine physicians, pediatricians, thoracic surgeons, general practitioners, junior doctors, nurses, physiotherapists, pharmacists, dietitians, pulmonary function and respiratory therapists, scientists and other healthcare providers who specialize or have an interest in respiratory disease and care throughout Ireland - North and South. It is self-governing and not affiliated with any regulatory body. It was established by a (then) junior doctor in 2008 and no demonstration/evidence of expertise is required for membership.
 W
WAn iron lung, also known as a tank ventilator or Drinker tank, is a type of negative pressure ventilator (NPV); a mechanical respirator which encloses most of a person's body, and varies the air pressure in the enclosed space, to stimulate breathing. It assists breathing when muscle control is lost, or the work of breathing exceeds the person's ability. Need for this treatment may result from diseases including polio and botulism and certain poisons.
 W
WA liquid ventilator is similar to a medical ventilator except that it should be able to ensure reliable total liquid ventilation with a breatheable liquid ·. Liquid ventilators are prototypes that may have been used for animal experimentations but experts recommend continued development of a liquid ventilator toward clinical applications.
 W
WLung volumes and lung capacities refer to the volume of air in the lungs at different phases of the respiratory cycle.
 W
WMechanical power is a medical term which is a measure of the amount of energy imparted to a patient by a mechanical ventilator.
 W
WMinute ventilation is the volume of gas inhaled or exhaled from a person's lungs per minute. It is an important parameter in respiratory medicine due to its relationship with blood carbon dioxide levels. It can be measured with devices such as a Wright respirometer or can be calculated from other known respiratory parameters. Although minute volume can be viewed as a unit of volume, it is usually treated in practice as a flow rate. Typical units involved are 0.5 L × 12 breaths/min = 6 L/min.
 W
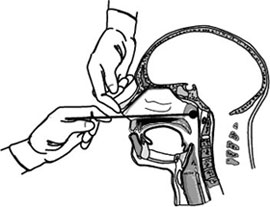
WA nasopharyngeal swab is a method for collecting a clinical test sample of nasal secretions from the back of the nose and throat. The sample is then analyzed for the presence of organisms or other clinical markers for disease. This diagnostic method is commonly used in suspected cases of whooping cough, diphtheria, influenza, and various types of diseases caused by the coronavirus family of viruses, including SARS, MERS, and COVID-19.
 W
WIn medicine, a nebulizer or nebuliser is a drug delivery device used to administer medication in the form of a mist inhaled into the lungs. Nebulizers are commonly used for the treatment of asthma, cystic fibrosis, COPD and other respiratory diseases or disorders. They use oxygen, compressed air or ultrasonic power to break up solutions and suspensions into small aerosol droplets that are inhaled from the mouthpiece of the device. An aerosol is a mixture of gas and solid or liquid particles.
 W
WObstructive lung disease is a category of respiratory disease characterized by airway obstruction. Many obstructive diseases of the lung result from narrowing (obstruction) of the smaller bronchi and larger bronchioles, often because of excessive contraction of the smooth muscle itself. It is generally characterized by inflamed and easily collapsible airways, obstruction to airflow, problems exhaling and frequent medical clinic visits and hospitalizations. Types of obstructive lung disease include; asthma, bronchiectasis, bronchitis and chronic obstructive pulmonary disease (COPD). Although COPD shares similar characteristics with all other obstructive lung diseases, such as the signs of coughing and wheezing, they are distinct conditions in terms of disease onset, frequency of symptoms and reversibility of airway obstruction. Cystic fibrosis is also sometimes included in obstructive pulmonary disease.
 W
WAn open-source ventilator is a disaster-situation ventilator made using a freely licensed (open-source) design, and ideally, freely available components and parts. Designs, components, and parts may be anywhere from completely reverse-engineered or completely new creations, components may be adaptations of various inexpensive existing products, and special hard-to-find and/or expensive parts may be 3D-printed instead of purchased. As of early 2020, the levels of documentation and testing of open-source ventilators was well below scientific and medical-grade standards.
 W
WAn oxygen firebreak, also known as a fire stop valve or fire safety valve, is a thermal fuse designed to extinguish a fire in the delivery tube being used by a patient on oxygen therapy and stop the flow of oxygen if the tube is accidentally ignited. Oxygen firebreaks are fitted into the oxygen delivery tubing close to the patient, typically around the patient's sternum where the two nasal cannula tubes join and connect to the delivery tubing.
 W
WAn oxygen mask provides a method to transfer breathing oxygen gas from a storage tank to the lungs. Oxygen masks may cover only the nose and mouth or the entire face. They may be made of plastic, silicone, or rubber. In certain circumstances, oxygen may be delivered via a nasal cannula instead of a mask.
 W
WAn oxygen tent consists of a canopy placed over the head and shoulders, or over the entire body of a patient to provide oxygen at a higher level than normal. Some devices cover only a part of the face. Oxygen tents are sometimes confused with altitude tents as used by athletes and those looking to acclimatize to a higher altitude, but those contain a reduced oxygen content.
 W
WOxygen therapy, also known as supplemental oxygen, is the use of oxygen as a medical treatment. This can include for low blood oxygen, carbon monoxide toxicity, cluster headaches, and to maintain enough oxygen while inhaled anesthetics are given. Long-term oxygen is often useful in people with chronically low oxygen such as from severe COPD or cystic fibrosis. Oxygen can be given in a number of ways including nasal cannula, face mask, and inside a hyperbaric chamber.
 W
WThe peak expiratory flow (PEF), also called peak expiratory flow rate (PEFR), is a person's maximum speed of expiration, as measured with a peak flow meter, a small, hand-held device used to monitor a person's ability to breathe out air. It measures the airflow through the bronchi and thus the degree of obstruction in the airways. Peak expiratory flow is typically measured in units of liters per minute (L/min).
 W
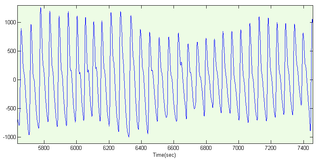
WA photoplethysmogram (PPG) is an optically obtained plethysmogram that can be used to detect blood volume changes in the microvascular bed of tissue. A PPG is often obtained by using a pulse oximeter which illuminates the skin and measures changes in light absorption. A conventional pulse oximeter monitors the perfusion of blood to the dermis and subcutaneous tissue of the skin.
 W
WA plethysmograph is an instrument for measuring changes in volume within an organ or whole body. The word is derived from the Greek "plethysmos", and "graphos".
 W
WPulmonary function testing (PFT) is a complete evaluation of the respiratory system including patient history, physical examinations, and tests of pulmonary function. The primary purpose of pulmonary function testing is to identify the severity of pulmonary impairment. Pulmonary function testing has diagnostic and therapeutic roles and helps clinicians answer some general questions about patients with lung disease. PFTs are normally performed by a respiratory therapist, physiotherapist, pulmonologist, and/or general practitioner.
 W
WPulmonary interstitial emphysema (PIE) is a collection of air outside of the normal air space of the pulmonary alveoli, found instead inside the connective tissue of the peribronchovascular sheaths, interlobular septa, and visceral pleura. This collection of air develops as a result of alveolar and terminal bronchiolar rupture. Pulmonary interstitial emphysema is more frequent in premature infants who require mechanical ventilation for severe lung disease. Infants suffering from pulmonary interstitial emphysema are typically recommended for admission to a neonatal intensive care unit.
 W
WA registered respiratory therapist (RRT) is another title for Respiratory Care Practitioners. In the United States, you must obtain a degree in Respiratory Care and must then sit for the board exams to become a RRT. RRT is issued by the National Board for Respiratory Care after passing the Therapist Multiple-Choice Examination NBRC-TMC and Clinical Simulation Examination NBRC-CSE examinations. Eligibility for the NBRC-CSE examination is based on scoring high enough on the NBRC-TMC, and holding at least an Associate of Science in Respiratory Care. In Canada the RRT certification is granted by examination from the Canadian Society of Respiratory Therapists. Internationally, respiratory care is governed by local governments and certification or license to practice as a respiratory practitioner is managed locally without the use of separate organizations as in the United States and Canada.
 W
WA respiratory pressure meter measures the maximum inspiratory and expiratory pressures that a patient can generate at either the mouth (MIP and MEP) or inspiratory pressure a patient can generate through their nose via a sniff manoeuvre (SNIP). These measurements require patient cooperation and are known as volitional tests of respiratory muscle strength. Handheld devices displaying the measurement achieved in cmH2O and the pressure trace created, allow quick patient testing away from the traditional pulmonary laboratory and are useful for ward based, out patient, and preoperative assessment as well as for use by pulmonologists and physiotherapists.
 W
WRheotrauma is a medical term for the harm caused to a patient's lungs by high gas flows as delivered by mechanical ventilation. Although mechanical ventilation may prevent death of a patient from the hypoxia or hypercarbia which may be caused by respiratory failure, it can also be damaging to the lungs, leading to ventilator-associated lung injury. Rheotrauma is one of the ways in which mechanical ventilation may do this, alongside volutrauma, barotrauma, atelectotrauma and biotrauma. Attempts have been made to combine all of the mechanical forces caused by the ventilator on the patient's lungs in an all encompassing term: mechanical power.
 W
WThe SensorMedics High-Frequency Oscillatory Ventilator is a patented high-frequency mechanical ventilator designed and manufactured by SensorMedics Corp. of Yorba Linda, California. After a series of acquisitions, Vyaire Medical, Inc. marketed the product as 3100A/B HFOV Ventilators. Model 3100 received premarket approval from the United States Food and Drug Administration (FDA) in 1991 for treatment of all forms of respiratory failure in neonatal patients. In 1995, it received pre-market approved for Pediatric Application with no upper weight limit for treating selected patients failing on conventional ventilation.
 W
WSpirometry is the most common of the pulmonary function tests (PFTs). It measures lung function, specifically the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled. Spirometry is helpful in assessing breathing patterns that identify conditions such as asthma, pulmonary fibrosis, cystic fibrosis, and COPD. It is also helpful as part of a system of health surveillance, in which breathing patterns are measured over time.
 W
WTidal volume is the lung volume representing the normal volume of air displaced between normal inhalation and exhalation when extra effort is not applied. In a healthy, young human adult, tidal volume is approximately 500 ml per inspiration or 7 ml/kg of body mass.
 W
WTracheal intubation, usually simply referred to as intubation, is the placement of a flexible plastic tube into the trachea (windpipe) to maintain an open airway or to serve as a conduit through which to administer certain drugs. It is frequently performed in critically injured, ill, or anesthetized patients to facilitate ventilation of the lungs, including mechanical ventilation, and to prevent the possibility of asphyxiation or airway obstruction.
 W
WUnderstanding Lung Sounds 3rd edition (2002) by Steven Lehrer is a book and audio CD that guides the student through the skills of lung auscultation. It provides a complete overview of lung examination, anatomy, physiology, and pathology. The audio CD presents and explains normal and abnormal lung sounds.
 W
WA ventilator is a machine that provides mechanical ventilation by moving breathable air into and out of the lungs, to deliver breaths to a patient who is physically unable to breathe, or breathing insufficiently. Modern ventilators are computerized microprocessor-controlled machines, but patients can also be ventilated with a simple, hand-operated bag valve mask. Ventilators are chiefly used in intensive-care medicine, home care, and emergency medicine and in anesthesiology.
 W
WIn physics, the Young–Laplace equation is a nonlinear partial differential equation that describes the capillary pressure difference sustained across the interface between two static fluids, such as water and air, due to the phenomenon of surface tension or wall tension, although use of the latter is only applicable if assuming that the wall is very thin. The Young–Laplace equation relates the pressure difference to the shape of the surface or wall and it is fundamentally important in the study of static capillary surfaces. It is a statement of normal stress balance for static fluids meeting at an interface, where the interface is treated as a surface :
 W
W W
W W
W W
W W
W W
W W
W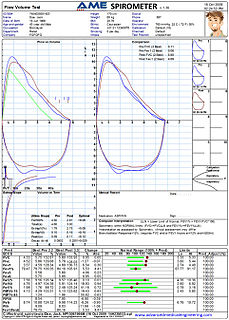 W
W